Click here to download this post
Dr. Nicholas L. DePace, M.D., F.A.C.C.
The main risk factor for atherosclerosis or hardening of the arteries is usually aging.
The older one gets the more likely they are to have atherosclerosis or hardening of the arteries and complications, such as stroke and heart attack.
In addition, in regard to the nervous system, specifically the Autonomic Nervous System (ANS), there is also a significant risk factor for malfunction with degeneration of nerve fibers; including due to a lack of a proper blood supply to the very delicate fibers.
This is a delicate interaction.
The ANS, specifically the Sympathetic branch of the ANS, controls the vasculature and thereby proper blood profusion of the various tissues.
It is the Parasympathetic branch of the ANS that senses tissue perfusion and drives the Sympathetics to that end. Normal, natural aging processes cause declines in the Parasympathetic and Sympathetic (P&S) Nervous Systems.
Chronic disease and other chronic condition that cause oxidative stress, accelerate these declines.
Reduced P&S activity to the vasculature reduces blood perfusion, which accelerates the aging of the nerves and tissues, which further reduces blood perfusion, and so goes the circle.
Unfortunately, this is asymptomatic for up to two decades before patients feel it; at which time it is very late in the progression.
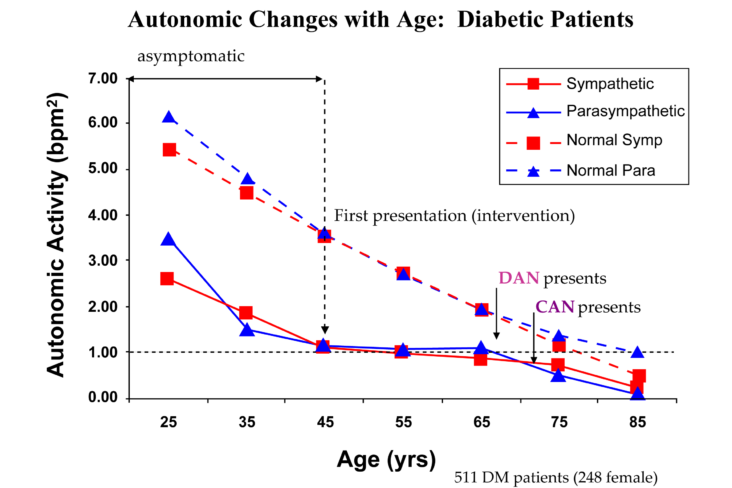
See the figure below comparing 300 healthy subjects over time and 500 chronic disease subjects over the same time.
Notice that the upper curves show a gradual decline over time in the healthy subjects. The lower curves show a more rapid decline in the chronic subjects, then the decline virtually stops once the patients comply with therapy.
Note, however, that the virtual stop occurs just above the horizontal broken line that indicates Cardiovascular Autonomic Neuropathy (CAN) which is end stage autonomic dysfunction and increased mortality risk (a 50% greater chance of heart attack or stroke in the next two years as compared with age-matched patients not demonstrating CAN). Note, DAN is the abbreviation for Diabetic Autonomic Neuropathy (also known as Advanced Autonomic Dysfunction in non-Diabetics). DAN is the precursor to CAN.

Eventually, age catches up with the chronic subjects and their decline parallels the healthy subjects with one important difference.
For the healthy subjects the Parasympathetics are a little higher than the Sympathetics. This is reversed in the chronic subjects.
A little more Parasympathetic activity in the geriatric population is known to be cardio-protective and is associated with lower morbidity and mortality risks.
The more Sympathetic activity in the older chronic patients is associated with greater numbers of co-morbidities (25% more), prescribed pharmaceuticals (37% more), and life-threatening risks (e.g., Major Cardiovascular Adverse Events, or MACE, 18% more).
In addition, with aging we see more small fiber inflammation and subsequent decrease in density of small fibers, which carry sensory pain and autonomic impulses. For both P&S decline and small fiber decline, early intervention often slows, significantly, the decline of nerve function (see figure below).
In the case of the P&S Nervous Systems, early interventions may return a patient to the normal path and perhaps buy back up to 20 years.

Vascular aging causes degeneration and hardening of the arteries and degeneration of the nerve fibers which ultimately affect every organ creating end-organ changes; particularly, the heart, brain and kidneys are very susceptible.
In general, age dependent injury to the vasculature and the nerve fibers becomes more manifested in the fifth or sixth decade of life.
However, some people develop this more prematurely, such as diabetics or individuals with high genetic lipid disorders, or other genetic disorders.
Some individuals have aging of their fibers and blood vessels more rapidly than other and, therefore, their biological age progresses faster than their chronological age.
There are certain noninvasive tests and blood test and biomarkers that can assess how the aging process is progressing.
Perhaps, the most well known is the length of the telomeres. Telomeres are repetitions of DNA sequences that protect the end of chromosomes.
With each cell division, the telomere is shortened and at such a point when they get below a critical length cells will be susceptible to death.
As a telomere is shortened, one can get a higher incidence of heart disease, coronary artery disease, and cerebral vascular disease.
Other mechanisms, such as DNA methylation and low-grade inflammation may accelerate the aging process.
The most common inflammation marker that we measure is C-reactive protein. Interleukin-6 is also another factor, which can be measure and be reflective of increased biological aging.
However, there is no one blood test that can indicate whether an individual’s nervous system or vascular system is aging prematurely or more rapidly.
Recently, the leaky gut disorder has become a very popular topic and has been associated with many changes in the ANS and malfunction and degeneration of the ANS.
Gut or gastrointestinal dysbiosis (microbial imbalance) has been linked to increase mortality risk and to disease.
Increased gut permeability alters the microbiotic composition; that is the composition of one’s intrinsic bacteria in their GI tract.
Toxic metabolites, if they leak through the cell junctions, can enter the blood stream and cause significant damage to blood vessels and nerves in the long term.
Breath tests and various urine tests after ingesting specific compounds can detect Chronic Intestinal Bacterial Overgrowth (CIBO) syndromes which if not corrected can be detrimental to vascular and neural structures.
Many noninvasive tests can assess whether one’s vascular system or neural system is prematurely aging.
We particularly like to assess HRV testing modalities especially coupled with respiration to assess Parasympathetic and Sympathetic power.
Sudomotor testing can assess small fiber integrity, inflammation and deficiency.
Carotid intimal thickness measures the thickness inside the carotid arteries and can also assess plaque burden, volume and density, which can be a surrogate for atherosclerosis and vascular aging.
Endothelial dysfunction, which can be derived from measures of ultrasound flow-mediated dilatation, or other similarly noninvasive techniques, which are easily available to clinicians in a laboratory and can demonstrate a malfunction of the small cells lining the arteries as one ages.
Calcium phosphate crystals deposited in the inner layer of the artery or the arterial intima, which is related to atherosclerosis, can be assessed with various tests.
Commonly used is a CT scan of the heart in which one calculates your Coronary Artery Calcium Score (CACS).
These are tests that can be obtained quite inexpensively and give a scoring system and assess the risk of future cardiac events and your degrees of potential atherosclerotic burden.
This test correlates well with coronary artery plaque burden.
Tests that measure arterial stiffness and velocity in the arteries, such as carotid-to-femoral pulse wave velocity or brachial-to-ankle pulse wave velocity can give an indication of how stiff the arteries are and how they are aging.
A high pulse wave velocity increases risk of cardiovascular disease and mortality from other causes.
Hypertension can promote arterial aging and rigidity as can high cholesterol, sedentary lifestyle and poor diet, such as high meats and saturated fats, high salt intake and high refined sugars.
Cigarette smoking is also a major culprit. While alcohol in low quantities may be protective for vascular endothelium, high quantities can be deleterious and can accelerate vascular aging.
Sleep habits are also important in regard to aging of the blood vessels and nerves in the body.
We strongly promote a Mediterranean diet with high fruits and vegetables, nuts, seeds and legumes, and moderate alcohol consumption with flavonoids and antioxidants, such as with wine products, omega-3 intake with fish.
In fact, omega-3 and fish oils have been shown to potentially decrease telomere length shortening and may have significant anti-aging properties.
There are many natural behavioral and pharmacological strategies which have anti-aging potential on the nerve fibers and blood vessels.
Behavioral strategies include moderate alcohol consumption, exercise 150-200 minutes a week, weight reduction, diet high in antioxidant contents such as the Mediterranean diet and even supplements with antioxidant properties such as Alpha Lipoic Acid, which is extremely beneficial to nerve fibers, specifically autonomic nervous system fibers, or small C fibers.
Cofactors with methylfolate and B vitamins are extremely beneficial also in preserving small fibers and even regenerating growth of them when they are deficient.
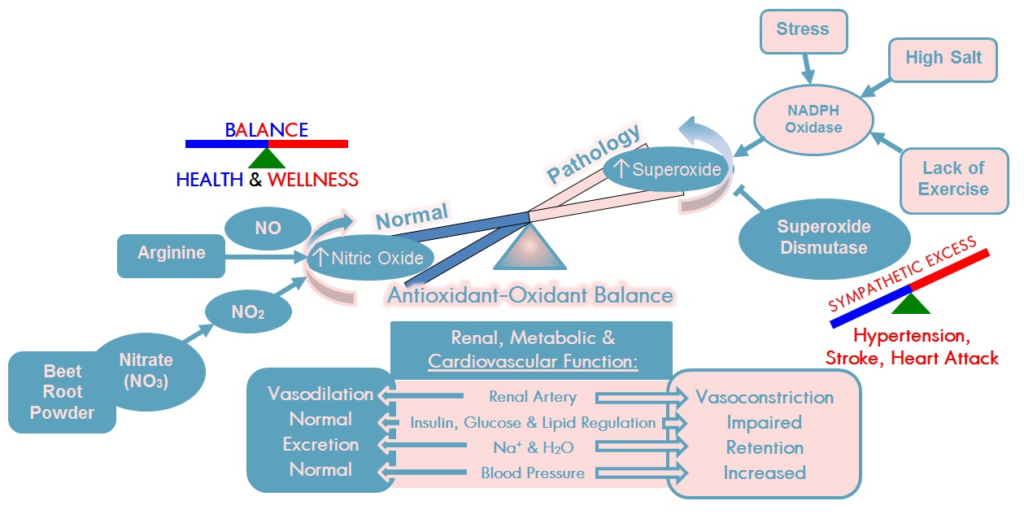
We have used Beetroot, L-arginine and L-citrulline as nitric oxide-producing compounds to better enhance endothelial function and preserve endothelial integrity and keep the blood vessels healthy.
These produce nitric oxide by various mechanisms.
As one ages, nitric oxide declines in a linear fashion, which is detrimental to the blood vessels.
High vegetable and fruit intake is also associated with improving endothelial function and decreased arterial stiffness and decreased blood pressure.
Other studies have shown arterial function is less stiff and improves with flavonoids and cocoa, tea, coffee and wine, also in fermented dairy products, nut, seeds and vegetables.
Olive oil and monosaturated fat has been shown to be extremely beneficial as an anti-inflammatory agent and endothelial-improving agent.
Key pathways to be regulated in the aging process that should be targeted are the mechanistic target of Rapamycin (mTOR) and Adenosine Monophosphate Activated Protein Kinase (AMPK). By inhibiting the mTOR and activating the AMPK, arterial stiffness can improve and blood pressure control can become better.
Regular moderate exercise to strengthen bone helps to keep calcium in the bone and reduce the calcium in arteries which reduces atherosclerosis, thereby reducing arterial stiffness.
Vitamin K2 (not ‘K’ but ‘K2’) is a new consideration in the anti-aging process.
Vitamin K2 works to redirect calcium from the soft tissue (e.g., arteries) to hard tissue (e.g., bones).
However, you must check with your physician to ensure that you are not at risk for blood clots. Vitamin K2 may increase the risk of blood clots.
Metformin is one of the most prescribed medicines for diabetes.
It has antioxidant effects in addition. Besides increasing insulin sensitivity, Metformin beneficially activates AMPK and beneficially inhibits mTOR.
Endothelial function, vascular stiffness and carotid artery calcium have been improved with Metformin.
Metformin has cardiovascular mortality benefits independent of its blood sugar lowering results. In addition, there has been data to suggest it can prevent certain types of cancer such as colon cancer.
Perhaps the best agent to prevent cancers is the Mediterranean diet which has been purported to reduce at least 16 types of cancer. Resveratrol is a polyphenol naturally present in grapes and berries and especially red wines.
It also activates AMPK and inhibits the mTOR pathways and has been very beneficial in protecting blood vessels and with antioxidant effects protecting nerve fibers.
In animal substances, Nicotinamide Adenine Dinucleotide has been shown to have anti-aging effects on the blood vessels.
Anti-inflammatory agents are being developed to beneficially affect nerve fibers and blood vessels.
More research is needed in that area.
One of the most unappreciated anti-inflammatory agents are Omega-3 fatty acids, such as from or fish or krill oils; especially the compound Eicosapentaenoic Acid (EPA) in fish oils can reduce heart attacks and strokes, up to 25% as found in one study; even on top of statin therapy.
Gut dysbiosis contributes to inflammation and abnormalities of the ANS and the vascular system.
Probiotics have been suggested as being useful in regulating gut dysbiosis as has certain antibiotics.
Risk reduction medicines used in heart disease, such as Aspirin, Statins, and Renin Angiotensin System blockers may have additional anti-aging potential.
Stress reduction and good sleep habits have significant effects on reducing oxidative stress and improving nerve fiber function and reducing degeneration of nerve fibers and improving blood pressure, endothelial function and arterial stiffness.
Relaxation techniques, such as meditation and yoga have been found to be extremely important in this regard.
We specifically use what we consider therapeutic quantities of Alpha Lipoic Acid, L-carnitine, and Co-enzyme Q10 in treating many of our patients with autonomic dysfunction and have found improvement in autonomic neuropathy testing parameters over a period of six months in these patients in our laboratory.
By combining these antioxidants, which we consider a Mitochondrial cocktail, as they produce more ATP energy molecules in addition to being good antioxidants, with Nitric Oxide producing compounds in appropriate concentrations (L-arginine, L-citrulline and Beetroot Extract), we believe we keep both the nerve fibers and arterial/vascular vessels from degenerating and aging. By lowering LDL cholesterol below 70 and by keeping LDL molecules from being oxidized with the use of antioxidants, by exercising and weight reduction to raise beneficial HDL levels, the vacuum cleaner of the blood vessels, we believe that we can affect reversal of Atherosclerosis in many patient’s especially when anti-inflammatory agents, such as statins (Rosuvastatin) is added in selected instances.
One needs to discuss all of these ideas and concepts with their personal physician who knows their case in detail to recommend what lifestyle, dietary, and pharmacological supplement and other additions or alterations in their regimen need to be done.
About the Author
Nicholas L. DePace, MD, FACC is a board-certified cardiologist and Medical Director of Franklin Cardiovascular Associates. A graduate of the Mount Sinai School of Medicine, Dr. DePace has decades of clinical, academic, and research experience and has held faculty appointments as a Clinical Professor of Medicine, becoming one of the youngest full professors in Philadelphia at the time of his appointment.
Dr. DePace specializes in the diagnosis and treatment of autonomic nervous system dysfunction (dysautonomia), including POTS, autonomic dysfunction associated with Ehlers-Danlos syndrome (EDS), chronic fatigue, and anxiety-like conditions that are frequently misdiagnosed. He is nationally recognized for his work on parasympathetic and sympathetic (P&S) nervous system imbalance, a core mechanism underlying many complex chronic disorders.
In addition to treating patients from across the United States, Dr. DePace is a prolific clinical researcher and author of multiple nationally distributed medical textbooks published by Springer and W.W. Norton, focusing on autonomic dysfunction, mitochondrial disorders, cardiovascular disease, and mind–body medicine.





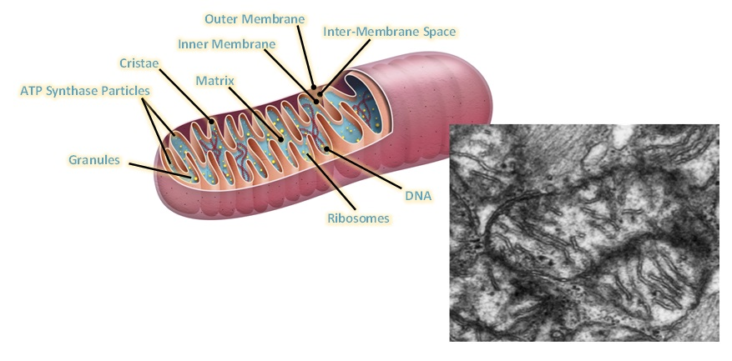
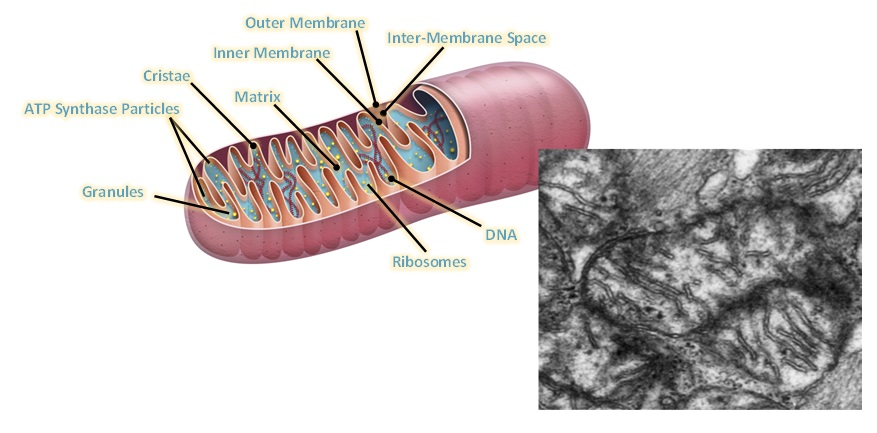 demonstrated. Urea Cycle dysregulation, Tricyclic Carboxylic Acid (TCA) Cycle disturbances, and dysregulation of Amino Acid metabolism are also involved. Also, gut microbiota disturbances have been identified. In regard to Mitochondrial dysfunction, studies state that ATP8 levels have been both noted to be reduced and elevated, and resting ATP8 synthesis rates have been variable. However, studies on isolated Peripheral Blood Mononuclear Cells have shown that under stress such as Hypoglycemia there is inefficient ATP8 production in Chronic Fatigue patients but not in normal controls. This was demonstrated by Tomas and coworkers in 2017. Therefore, while resting ATP studies show that production may not be significantly abnormal in ME/CFS patients as compared with controls, it appears that under stressful situations, such as Hypoglycemia, the situation is different when one analyzes peripheral blood mononuclear cell ATP production. ATP is the energy molecule of the cell and of the body and is produced in the Mitochondria, which are the energy factories of the body.
demonstrated. Urea Cycle dysregulation, Tricyclic Carboxylic Acid (TCA) Cycle disturbances, and dysregulation of Amino Acid metabolism are also involved. Also, gut microbiota disturbances have been identified. In regard to Mitochondrial dysfunction, studies state that ATP8 levels have been both noted to be reduced and elevated, and resting ATP8 synthesis rates have been variable. However, studies on isolated Peripheral Blood Mononuclear Cells have shown that under stress such as Hypoglycemia there is inefficient ATP8 production in Chronic Fatigue patients but not in normal controls. This was demonstrated by Tomas and coworkers in 2017. Therefore, while resting ATP studies show that production may not be significantly abnormal in ME/CFS patients as compared with controls, it appears that under stressful situations, such as Hypoglycemia, the situation is different when one analyzes peripheral blood mononuclear cell ATP production. ATP is the energy molecule of the cell and of the body and is produced in the Mitochondria, which are the energy factories of the body. Figure Legend: Schematic diagram showing various viral pathogens potentially associated with ME/CFS and possible molecular mechanisms altered by these pathogens that can contribute to ME/CFS development [[i]].
Figure Legend: Schematic diagram showing various viral pathogens potentially associated with ME/CFS and possible molecular mechanisms altered by these pathogens that can contribute to ME/CFS development [[i]].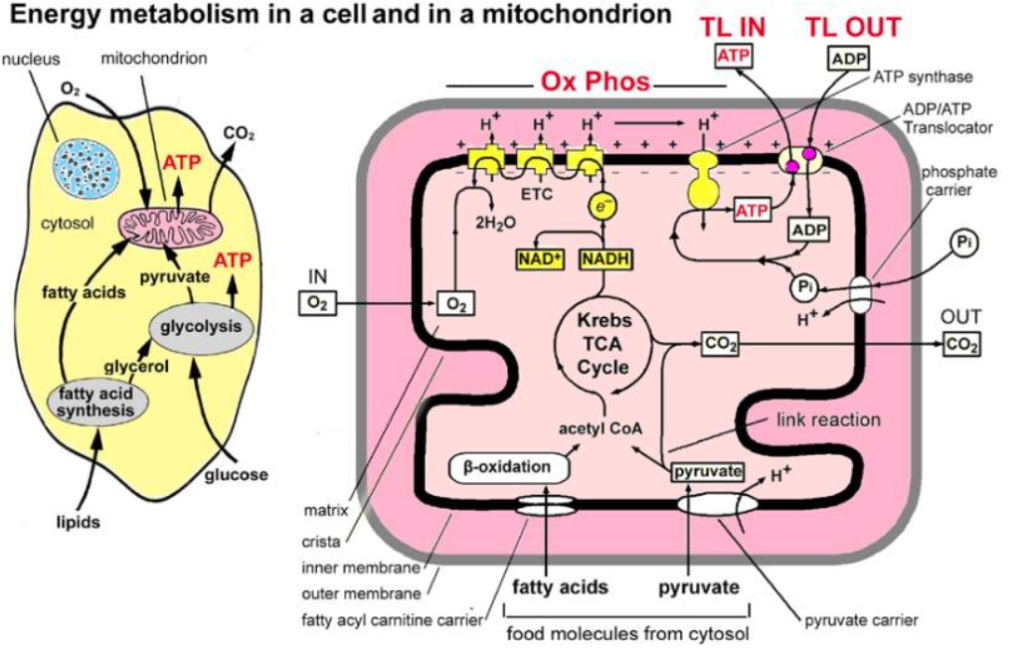

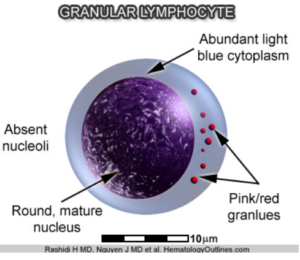 researched but has been performed on a subtype that is especially comorbid with Irritable Bowel Syndrome, which is seen in many Chronic Fatigue patients. Autoimmune evidence has been strengthened by the fact that there is a decrease in the natural killer cell cytotoxicity in patients with ME/CFS. Natural killer cells are Granular Lymphocytes which attack viruses and bacteria foreign to the body. In addition, the autoimmune evidence is supported by autoantibodies which have been noted against various transmitter receptors, both Muscarinic receptors and Beta receptors. A high incidence of these receptors has also been found in patients with Postural Orthostatic Tachycardia. Specifically, autoantibodies against the Muscarinic and Cholinergic receptors #3 (M3) and autoantibodies against the Muscarinic and Cholinergic receptor #4 M4) are elevated in 20-30% of all patients suffering from ME/CFS. Other studies have shown Beta-1 Adrenergic Receptor Autoantibodies and Beta-2 Adrenergic Receptor Autoantibodies along with Alpha-1 Adrenergic Receptor Autoantibodies, the same autoantibodies which we find in a significant number of patients with Postural Orthostatic Tachycardia Syndrome.
researched but has been performed on a subtype that is especially comorbid with Irritable Bowel Syndrome, which is seen in many Chronic Fatigue patients. Autoimmune evidence has been strengthened by the fact that there is a decrease in the natural killer cell cytotoxicity in patients with ME/CFS. Natural killer cells are Granular Lymphocytes which attack viruses and bacteria foreign to the body. In addition, the autoimmune evidence is supported by autoantibodies which have been noted against various transmitter receptors, both Muscarinic receptors and Beta receptors. A high incidence of these receptors has also been found in patients with Postural Orthostatic Tachycardia. Specifically, autoantibodies against the Muscarinic and Cholinergic receptors #3 (M3) and autoantibodies against the Muscarinic and Cholinergic receptor #4 M4) are elevated in 20-30% of all patients suffering from ME/CFS. Other studies have shown Beta-1 Adrenergic Receptor Autoantibodies and Beta-2 Adrenergic Receptor Autoantibodies along with Alpha-1 Adrenergic Receptor Autoantibodies, the same autoantibodies which we find in a significant number of patients with Postural Orthostatic Tachycardia Syndrome.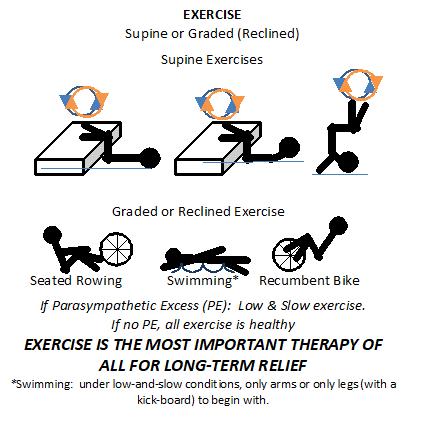

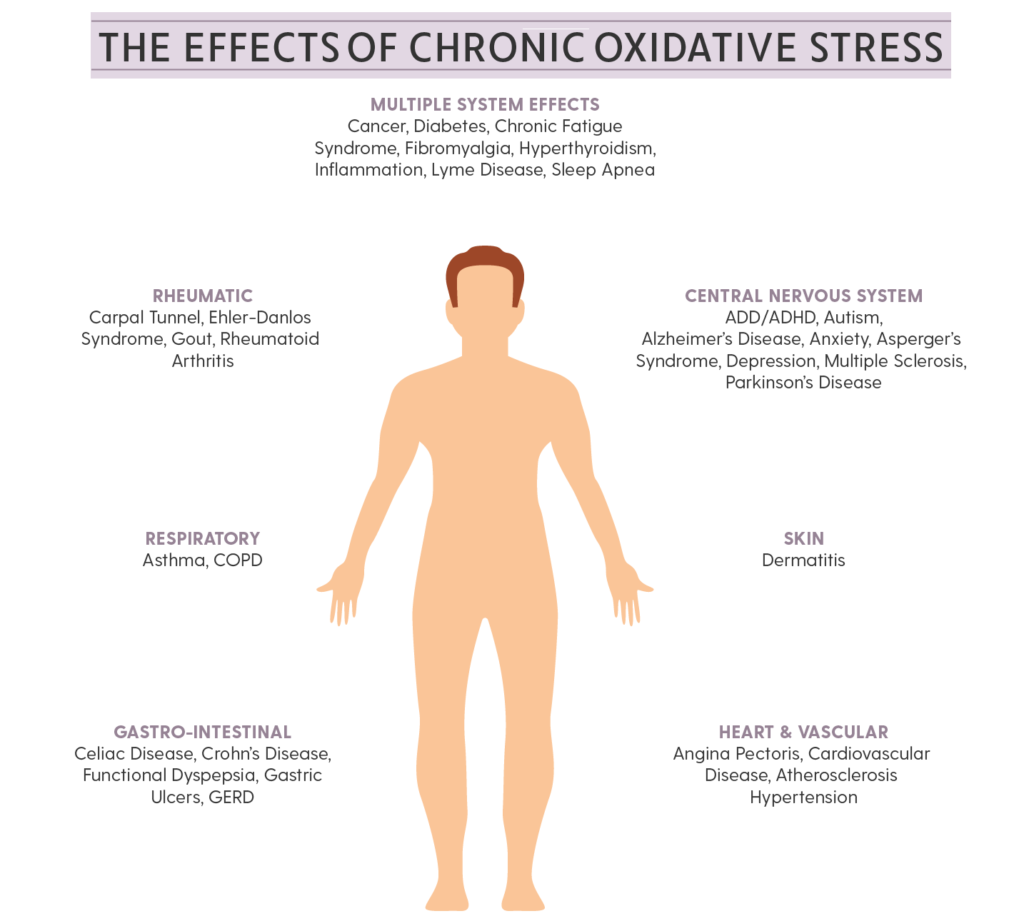
 The body has natural Antioxidants to sequester, or neutralize, Free Radicals to prevent oxidative stress from injuring tissues and destroying cells. Natural Antioxidants include Vitamins A, C, & E, Glutathione, Selenium, Alpha Lipoic Acid (ALA) and Coenzyme Q-10 (CoQ10). Many scientists feel that ALA is the ideal antioxidant because it is both a lipid and water soluble (it can dissolve in both lipid and water environments) and can cross the Blood-Brain Barrier. It is absorbed rapidly through the Gastrointestinal (GI) tract high up in the digestive system and it is immediately available to neutralize free radicals quickly. It has also been shown to recycle Vitamin C and Vitamin E in the body. Vitamin C is only water soluble and Vitamin E is only lipid soluble. Because ALA is both liquid and lipid soluble, it can pass the Blood-Brain Barrier and increase available brain energy. Not only can ALA recycle Vitamin C & E but also Glutathione. Glutathione is probably the most important intracellular Antioxidant.
The body has natural Antioxidants to sequester, or neutralize, Free Radicals to prevent oxidative stress from injuring tissues and destroying cells. Natural Antioxidants include Vitamins A, C, & E, Glutathione, Selenium, Alpha Lipoic Acid (ALA) and Coenzyme Q-10 (CoQ10). Many scientists feel that ALA is the ideal antioxidant because it is both a lipid and water soluble (it can dissolve in both lipid and water environments) and can cross the Blood-Brain Barrier. It is absorbed rapidly through the Gastrointestinal (GI) tract high up in the digestive system and it is immediately available to neutralize free radicals quickly. It has also been shown to recycle Vitamin C and Vitamin E in the body. Vitamin C is only water soluble and Vitamin E is only lipid soluble. Because ALA is both liquid and lipid soluble, it can pass the Blood-Brain Barrier and increase available brain energy. Not only can ALA recycle Vitamin C & E but also Glutathione. Glutathione is probably the most important intracellular Antioxidant.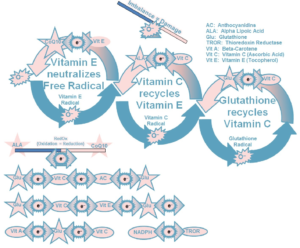 Antioxidant and is synthesized within the Mitochondria and consists of three Amino Acids, Cysteine, Glutamic Acid, and Glycine. Glutathione is not easily absorbed orally and cannot pass through the Mitochondrial membrane so easily. Therefore, anything that preserves the body’s natural production of Glutathione and keeps the concentration up is valuable. This is where ALA comes in as a very important Antioxidant. It recycles Glutathione and replenishes the body’s stores. Glutathione is a very important component of several enzyme systems in the body that are organ-protective from disease. There is some data to suggest that ALA is also an excellent chelating agent and protects us from heavy metals, although this is beyond the scope of this discussion.
Antioxidant and is synthesized within the Mitochondria and consists of three Amino Acids, Cysteine, Glutamic Acid, and Glycine. Glutathione is not easily absorbed orally and cannot pass through the Mitochondrial membrane so easily. Therefore, anything that preserves the body’s natural production of Glutathione and keeps the concentration up is valuable. This is where ALA comes in as a very important Antioxidant. It recycles Glutathione and replenishes the body’s stores. Glutathione is a very important component of several enzyme systems in the body that are organ-protective from disease. There is some data to suggest that ALA is also an excellent chelating agent and protects us from heavy metals, although this is beyond the scope of this discussion.