Click here to download this post
LIGHTHEADEDNESS*, SEVERE FATIGUE, “BRAIN FOG,” AND AN INABILITY TO FUNCTION
MAY BE DUE TO ORTHOSTATIC INTOLERANCE
* Doctors separate lightheadedness and dizziness. Dizziness is reserved for balance problems due to Vestibular dysfunction. Lightheadedness describes all other types of dizziness.
Patients often present to our Autonomic Dysfunction (Dysautonomia) practice with complaints of inability to stand for long periods of time, lack of energy, severe fatigue, an inability to perform common chores without exhaustion, “brain fog” and mental cloudiness with a frequent need to lie down. They complain of shortness of breath (SOB) but have normal structural hearts and lungs with abnormal venous pooling which creates a lack of cardiac output that may result in decreased exercise tolerance and the dyspnea, which includes SOB. They also often complain of tachycardia, or fast heartbeat especially when standing. Many of these patients also have special types of watches which can record their heart rate, and they can demonstrate going well above 150 beats per minute, oftentimes with no activity and just standing.
Autonomic Dysfunction or Dysautonomia are the terms used to describe disorders with the Autonomic Nervous System. You may think of the Autonomic Nervous System as the “Automatic” Nervous System. It controls all the things you do not have to think about: eye-blink, digestion, blood pressure, heart rate, breathing; in fact, it is the portion of the nervous system that controls and coordinates all systems and cells of the body. It has two parts: the Parasympathetic and the Sympathetic (P&S) nervous systems. The P&S nervous systems are like the brakes and accelerator on a car. The Parasympathetics are like the brakes and the Sympathetics are like the accelerator.
Standing up or sitting up causes the heart to have to fight gravity to get blood to the head or even to the heart and everything above the heart. When the P&S nervous systems are not coordinating properly, the heart has to work too hard and this may cause lightheadedness. If this condition is permitted to linger and persist, it will lead to the fatigue, “brain fog,” and other symptoms listed above. Using the “brakes and accelerator” example, moving to the upright or standing position is like being at a red light.
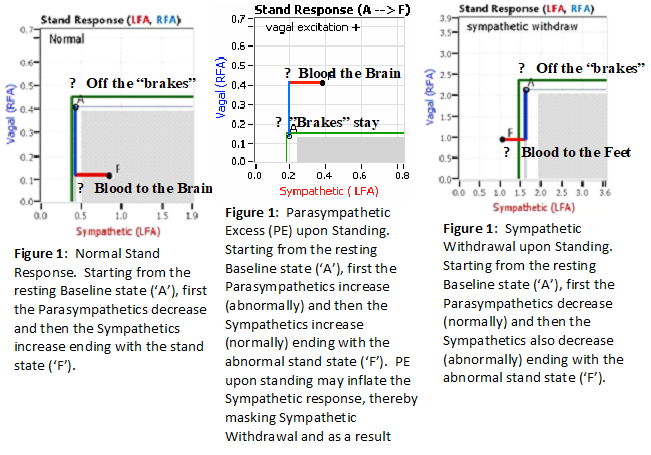
As in a car (with an automatic transmission), if you are at a red light with your foot on the brakes and the light turns green, what is the first thing you do? … You take your foot off the brakes. Even before you touch the accelerator, you begin to roll, you already begin to accelerate. Taking your foot off the brakes minimizes the amount gas (read that as adrenaline) and acceleration (read that as Sympathetic stress) you need to reach your desired speed. The P&S nervous systems normally act in much the same manner: first the Parasympathetics decrease to facilitate and minimize the Sympathetic response, and then the Sympathetics increase (see Figure 1) moving blood from the feet to the abdomen to help the heart pump blood to the brain.
One of two things may happen if this coordination does not occur properly. Either you do not take your foot off the brakes or you do not press the accelerator. If you do not take your foot off the brakes (we call this Parasympathetic Excess or PE) and then hit the accelerator, you still go (see Figure 2), but you must use much more gas (read that as “adrenaline”) and you must over-rev your engine (read that as “over stimulate the Sympathetics) to go anywhere. This places more wear (stress) on the engine and on the brakes. This is stress and effort while only standing still. It feels like you are running a marathon while you are only standing still. If you take your foot off the brakes, but do not press the accelerator (we call this Sympathetic Withdrawal or SW), then you do not go anywhere; read that the blood does not go anywhere (see Figure 3). The blood in your legs stays in your legs and feet making it hard for the heart to pump it to the brain. With just enough blood in the brain the brain “falls asleep” and fatigue and a mild depression results with the symptoms listed above and more.
Care from our practice is often sought out after individuals do research on the Internet and type in a search for “POTS” doctors, or dysautonomia. A lot of patients come to our clinic and they are not sure if the have actual POTS and want to know definitively. First know that the ‘O’ in POTS stands for “Orthostatic.” It is Greek for change (“ortho”) the same (“static”). In other words, when you stand (the change) everything should feel the same as if you were still sitting down; no lightheadedness (dizziness) or fatigue or racing heart, etc. One cause of Orthostatic dysfunction is SW, and Postural Orthostatic Tachycardia Syndrome is a form of Orthostatic dysfunction that may be based on SW with an excessive heart rates upon standing that brings with it mental fatigue and mental cloudiness.
Over years of observation and research, criteria were made to describe the POTS complex. POTS is not a disease but is a syndrome. This is because it has many causes and many presentations. Also, it is not so clear if one definitely has POTS or not POTS, but simply Orthostatic Intolerance where their heart rate does not rise significantly when they stand. However these not POTS (Orthostatic Intolerance) patients they still have symptoms of “brain fog,” mental cloudiness, and severe fatigue or chronic-fatigue-type syndromes. By definition, POTS occurs when the heart rate (1) in a very young person (< 18 yrs) rises more than 40 beats per minute (bpm) on standing, or (2) in a person over the age of 18 over the heart rate rises more than 30 bpm on standing. Oftentimes, in POTS patients, regardless of age, their (absolute) heart rate is 120 bpm or higher.
There are patients who do not reach the 120 bpm threshold when they stand, even after 10 minutes, nor do they have increases of 30 or 40 bpm when standing. Many of these patients, however, if tested in the early morning when they arise will meet the criteria and later in the day they have better compensation. Therefore, the time of day the testing is done is important. Early morning is more sensitive to picking up these dramatic heart rate increases in a patient.
The status of a patient’s hydration is important. If they are well hydrated the day they come to the office for an evaluation, they may not reach the heart rate thresholds that are definitive for the diagnosis of POTS. If they are poorly hydrated, or have not slept well, oftentimes they will have significant heart rate runs.
Sometimes patients will come to our office and test positive and other times negative for POTS. Also, medications that the patient takes can influence heart rate responses, even if they are unrelated to treating autonomic dysfunction. More importantly, deconditioning after a surgical procedure, for example, with bed rest also influences heart rate responses.
Whether the heart rate does meet the criteria and goes up 30-40 bpm with standing and does exceed 120 bpm routinely in a patient or not, does not necessarily mean that they do not have a postural orthostatic disorder. This is really a spectrum. A similar analogy would be a person who has a blood sugar of 120, fasting, compared to another person who has a blood sugar of 130, fasting. While the cutoff is 125 for a diagnosis of diabetes, a blood sugar of 120 is a borderline diabetic, or an insulin resistant person, and a person with 130, obviously meets the criteria. However, if we measure a three month index of diabetes such as a hemoglobin A1c, it may actually be higher than a person whose blood sugar fasting is only 120 compared to one who is 130, which means there are fluctuations long-term with the patient’s blood sugar. This is also the case in people with Orthostatic Intolerance syndrome and POTS.
While this may sound confusing, it really is not. Basically, if an individual’s heart rate does go up when they stand for a period of time, especially in the morning, and they have symptoms over a six month period or more consistent with brain fog, decreased cerebral perfusion, lightheadedness, fatigue and mental cloudiness, they qualify for a diagnosis of Orthostatic Intolerance. These patients often feel much better when lying down and worse when they stand or do minimal activity. Treatment may be the same for both subsets of patients. Rather than tell patients you do have POTS or not have POTS, we do tests confirm the diagnosis of POTS or Orthostatic Intolerance. The tests help us to see the features of your stand abnormalities. These features help to determine whether your symptoms are consistent with Orthostatic Intolerance syndrome, which may be a precursor of POTS, or a variation of POTS.
Before diagnosing POTS, or any Orthostatic Intolerance syndrome which cause a rise in heart rate when people are standing, one needs to exclude common causes that do this and are not related to a dysautonomia, such as anemia, hyperthyroidism, dehydration, fever, adrenal tumors and medication effect.
Females have a much higher incidence of having Orthostatic Intolerance and POTS syndrome than males. We believe this is related to smaller hearts, less left ventricular wall mass and perhaps some hormonal manipulation, since it is rare to find individual females who have POTS when they are post-menopausal. Also, POTS flare-ups occur during the time of menstrual periods, when blood volume may be reduced as well. This oftentimes offers us an opportunity to add pharmacology specifically during the menstrual cycle when patients are most symptomatic (we often order volume expanders, such as Florinef or desmopressin, or increase the Midodrine dose if one is already on Midodrine, which is a vasoconstrictor and not a volume expander).
POTS is associated with many other entities. Probably the mechanisms are unrelated, but we are not quite sure. For example, POTS is very common in individuals with fibromyalgia and migraines. It is also very common in people with Ehlers-Danlos syndrome, or hypermobility syndromes. Also, it is seen in patients with anxiety and hypervigilance. That is those patients who are very sensitive to stimuli such as touch, light, sound, and so forth. Chronic fatigue and fibromyalgia and brain fog have been associated with POTS. Most likely, many of these patient’s are misdiagnosed as fibromyalgia and indeed have just orthostatic intolerance symptoms with muscle aches especially coat hanger pain between the shoulder blades and neck. We do not like to use the label fibromyalgia in patients as it is over-utilized especially in patients with dysautonomia. Migraines are often associated with dysautonomia both in terms and sympathetic and parasympathetic problems, and identifying what is the mechanism may facilitate treatment of migraines.
Patients often ask me what type of POTS they have since there are different subtypes proposed. POTS patients most of the time may have what we consider as neuropathic POTS. Oftentimes, they have abnormal sudomotor or sweat test result, which reflect abnormal small nerve fibers in the periphery. Patients with neuropathic POTS have a type of sympathetic denervation in which the small nerves to the lower extremities do not work well and venous pooling results (SW). Their feet often turn a purplish color from venous pooling, and this is often seen even in the testing laboratory. Sometimes this purplish color is mistaken for Raynaud’s syndrome, but it occurs in the heat as well as the cold. Since it occurs in the heat as well (even though your feet are cold) means that it is not Raynaud’s syndrome.
Less common is the hyperadrenergic POTS. These patients will oftentimes show a significant hypertensive response on standing or on the tilt test. They will also have very elevated norepinephrine levels when tested in the morning in the stand position compared to the sitting position. Oftentimes the levels will exceed 600 pg/mL. This reflects an exaggerated sympathetic response. They also have increasing symptoms with exertion and emotional stress and increasing heart rates, which overshoot dramatically. Assessing their Valsalva, a response where one holds their breath and bears down in the testing lab, often will show an overshoot of their blood pressures or heart rates. These patients often respond better to beta-blocker, or adrenergic blocking agents, whereas the patients who show a neuropathic response often do better with alpha 1 constrictors which constrict the blood vessels such as Midodrine.
There is also a proposed volume depletion, or low volume types of POTS. There are people who appear to be chronically dehydrated and constantly urinating. So even if they drink plenty of water, they do not keep it in their systems to help their condition. These patient s respond better to desmopressin, or to Florinef, which keep or expand blood volume through the kidneys, more so than Midodrine or beta-blockers which work on the nerves. Over the long-term, we do not like to use Florinef because of myocardial fibrosis as a potential side effect. Therefore, we try to limit Florinef to the lowest dose and even use it only several times a week or during menstrual periods to minimize any side effects.
We can oftentimes get an idea if someone has a hypovolemic or low volume types of POTS by measuring a 24-urine to see if they have a urine value less than 100 mEq per liter. We may also do a spot urine to see if the urine sodium is low. It is estimated that 30% of POTS patients have evidence of low volume on 24-hour urine tests which show less than 100 mEq of urine sodium excretion in 24 hours, and they can have overlapping features with the other types of POTS subtypes.
Another proposed subtype is Mast Cell activation disorder which is often associated with flushing, shortness of breath, headache episodes, throat tightness, occasional anaphylactic reactions, hives and pruritus or itching. It is difficult to diagnosis this type of a disorder, but an elevated plasma tryptase during an acute episode or high levels of N-methylhistamine in the urine especially over 24 hours may be helpful along with other urine prostaglandin measurements.
Lastly, it has been proposed that autoimmune disorders may be responsible for POTS. We find this not to be the case at all, and rarely find cases of POTS with positive autoimmune antibodies. These are usually in patients who have positive histories in their family, collagen vascular disease such as Sjogren’s, lupus, rheumatoid arthritis or mixed connective tissue disease. Rarely do we find antibodies against adrenergic receptors and (muscarinic) acetylcholine receptors. The presence of ganglionic acetylcholine antibodies is occasionally seen and makes one suspect autoimmune cause. There is no data that any immuno-modulating agents, such as steroids or IVIG are helpful if this is found and rarely are these antibodies positive. At times, a paraneoplastic antibody workup is ordered, especially in people with suspected mast cell, and rarely are these positive. For completeness of workup though most centers will do these tests.
Therefore, is it important to determine what subtype of POTS a person may have? The answer is no. Treatment is basically very similar. We first start with lifestyle changes, which are the most important, especially exercise. There is no better treatment than a graded exercise program: starting in a reclined position then working up to an up-right position as your heart becomes more conditioned. This will build up your heart muscle mass and heart conditioning, whether you have POTS or other Orthostatic Intolerance states. From a heart or cardiac conditioning perspective, all Orthostatic dysfunctions are similar. Easy exercise over a prolonged period of time has been shown better to blunt the heart rate response and some of the Orthostatic Intolerance symptoms than beta-blockers such as Propranolol.
Propranolol is useful mostly for reducing the heart rate as do other beta-blockers. Usually, we like to use non-cardio-selective beta-blockers as they can also block beta2 receptors, which help to vasodilate (relax blood vessels and make it harder to pump blood to the heart and brain). Metoprolol is the least preferred of the beta-blockers. However, it is the most commonly prescribed. Propranolol in low doses and not high doses, in our experience and other centers, is the best agent to keep heart rate from going too high.
Midodrine is also very effective in constricting the veins in the lower extremities and promoting blood flow to the heart and then to the brain. Compression stockings are a major lifestyle improvement and so are abdominal binders. These garments will help move the blood from the lower extremities when the nerves and blood vessels are not. Fluid intake is a mainstay, 48-64 ounces a day is the minimal recommendation. We do recommend adding electrolyte (salt) solutions to them, especially flavored ones. However, you should stay away from any that include caffeine, sugar (including artificial sugar) or alcohol, because these all will dehydrate. Salt intake should be liberal at 6-8 grams a day, but spread out over the whole day, like nibbling on chips, pretzels, or salted nuts all day long. Many patients like to take special types of salt, such as sea salt or Himalayan salt. Leg crossing, squatting and other resistance-producing maneuvers have also been found to be important for temporizing for improvement in symptoms when one is standing and having difficulty with various symptoms, such as brain fog and dizziness (see Figure 4).
In terms of volume expanders, Florinef, as discussed, does expand volume initially, but is better used after a period of time just to sensitize the body to their own norepinephrine production. Low doses several times a week, or even during times of menstrual cycle, are preferred to avoid side effects, especially long-term side effects. Desmopressin we have found to be more useful having less side effects. Effectively, Desmopressin slows the production of urine so your body is better able to hydrate, especially if you are already drinking a lot of water (up to 64 oz per day) and all you seem to do is run to the bathroom and are still thirsty. Desmopressin is best taken at night. We usually start with 0.2 mg on Fridays once a week and oftentimes will increase it to twice a week. We do not like to use it every day because of its propensity to cause low sodium in the blood, and we do check the electrolytes after starting it. We like to use Desmopressin as an add-on to Midodrine to relieve symptoms, especially in patients who feel that hydration is very helpful or especially in patients who go to emergency rooms or urgent cares to get intravenous fluid infusions for relief at times when symptoms are disabling. We have put patients on Desmopressin at low dose and found that they require less or no infusions of intravenous fluids periodically for symptom relief.
Often as an add-on to Midodrine, we have used Mestinon, which is an acetylcholinesterase inhibitor and we believe is effective in beneficially affecting the autonomics. It is particularly helpful in patients with constipation-type symptoms or those who have anhidrosis or decreased sweating.
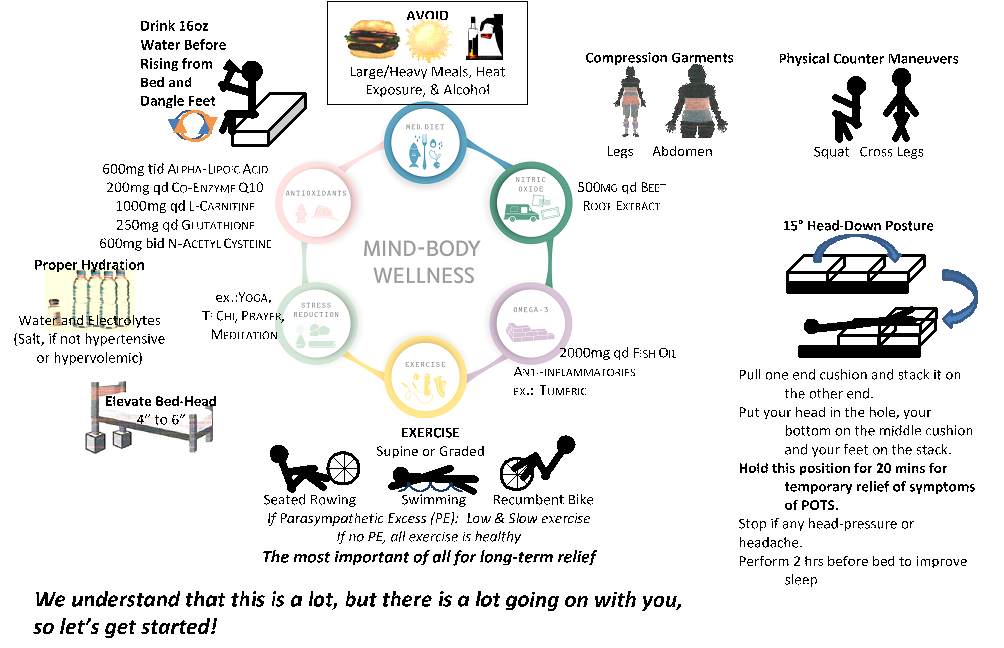
Figure 4: Postural Orthostatic Tachycardia Syndrome Algorithm
POTS, or Orthostatic Intolerance symptoms create a vicious cycle. Patients becomes tired and exercise less, and this makes a sedentary state similar to bed rest and makes the syndrome worse. Therefore, exercise programs at low level, especially with supine bicycle, swimming and rowing machines is preferred initially and one then graduates to an elliptical machine and eventually a treadmill. Low dose resistant exercises can be introduced later on in addition.
For patients who are totally bed-ridden (if they lift their head of the pillow they feel like they will faint) there are exercises that may be done in a totally supine position as in Figure 5. The exercise program should be done reclined or even supine with legs elevated. For example, as depicted (Figure 5, left), to start with, put your bottom against your bed (if not too tall, or a couch or something like that) and just move your lower legs like she was walking at 2 mph (like kicking the bed with your heals). Then you could graduate to more of a bicycling motion without the bed as depicted Figure 5, right. Then increase to lifting your head off the floor, as in Figure 5 center. Then increase to a full inverted bicycling activity as depicted in Figure 5, right. Of course with every transition or even as needed you may use your bed for support, while still moving your legs like walking at 2 mph. Eventually, as you become more conditioned you could do these exercises without your bed for support (“free standing”). Then move to reclined cycling, then up right cycling, then walking (as suggested in Figure 4); all the while continuing to move your legs like you would while walking at 2 mph. The goal is to build up to 40 minutes a day and maintain for at least 6 months.

Figure 5: Supine exercises to help build cardiac conditioning in POTS patients who cannot even sit for any length of time. From left to right, Left) inverted cycling flat on the floor with legs on the bed and lower legs moving, like walking at 2 mph, Center) similar to the previous, but with the head elevated and supported by your hands, and Right) a true inverted cycling exercise.
Things to avoid with POTS are heat, alcohol, and heavy meals since after a heavy meal blood is directed to the gut (the splanchnic circulation or the GI tract) and away from the brain. Importantly, one should in almost all incidents not take stimulant drugs, such as Adderall or Ritalin. Drugs that may increase heart rate such as tricyclics must be used cautiously and many times a beta-blocker must be used first. Medications such as Wellbutrin or norepinephrine reuptake inhibitors may also worsen POTS symptoms. High dose beta-blockers can worsen POTS symptoms, and we attempt to use the lowest dose as possible. When patients do not respond to beta-blockers we often go off-label and use Corlanor, which has hardly any side effects and is excellent in lowering heart rate at the sinus node for symptomatic relief of orthostatic tachycardias.
Many patients come to us already on Adderall or Ritalin or various stimulants. We attempt to use more physiologic based medications and lifestyle approaches and wean them from these medicines since we consider them more of a band-aid. While they can essentially stimulate the brain and reduce brain fog, their effects wear off and they have many side effects and can worsen the orthostatic tachycardia. There are some subsets of patients that rarely may benefit from these stimulant medications, but these are few and in only certain circumstances should this be allowed and testing needs to be done to be certain they do not have hyperadrenergic components to their POTS syndrome.
In regard to tilt testing, a full tilt test is not a good test to diagnose POTS syndrome but it is more appropriate to differentiate Vasovagal Syncope from Orthostatic Intolerance disorders. Vasovagal Syncope is known to be co-morbid (occur at the same time) as POTS or Orthostatic Intolerance. Physiologically, it is possible for both to occur. As discussed, Orthostatic dysfunction (i.e., POTS, Orthostatic Hypotension, and Orthostatic Intolerance) may be caused by SW. SW is an alpha-adrenergic or alpha-Sympathetic response (“adrenergic” and “Sympathetic” are synonyms). Syncope is a beta-adrenergic response. (In the autonomic nervous system there are the P&S nervous systems, and the P&S nervous systems have subsystems. In the case of the Sympathetics there are the alpha-adrenergics that largely innervate the blood vessels, and the beta-adrenergics that largely innervate the heart and the lungs.) So POTS and Syncope are mediated through two different parts of the nervous system, which both may be defective. Furthermore, the “Vasovagal” part is Parasympathetic (“Vagal” and “Parasympathetic” are synonymous). Therefore, POTS (or Orthostatic Intolerance) and Vasovagal Syncope are mediated through three different parts of the nervous system and all three may be defective and require treatment. Which may occur all in parallel.
A significant problem with tilt-testing is the standard procedure of giving medications during the tilt testing. This produces too many false-positives, and a normal response to some of these medicines, such as isoproterenol and nitroglycerin just elevate heart rate. Oftentimes, I will have patients come to me who have had tilt tests in electrophysiology labs or hospitals which show that their heart rates go very high after taking isoproterenol and nitroglycerin and are diagnosed with POTS syndrome. This is not correct. Normal individuals will have these responses also. One should be careful when using the results of tilt tests for any type of diagnosis of POTS or postural orthostatic syndromes.
I am often asked can POTS syndrome go into remission. The answer is yes, especially if an individual exercises for at least a six month period of time and oftentimes we can wean them off their medications. Of course, there are flare-ups over a period of time during periods of stress, dehydration, surgical procedures, concussions, motor vehicle accident, or bacterial or viral infections. Many times these are triggering events for the initial episode of POTS. However, we feel most patients can get significant improvement and even go into a remission phase. Also, during pregnancy many patients seem to improve with increase in plasma volume only to have a recurrence of their POTS symptoms after delivery and therefore they should be watched carefully post-delivery and treated appropriately, including caring for the infant regarding breast feeding.
Therefore, we recommend the following lifestyle changes in patients with Orthostatic Intolerance symptoms, or POTS (see Figure 4).
- Avoid alcohol.
- Avoid heat or sun or humid environments.
- Avoid heavy meals and eat six small meals a day, if possible.
- Learn how to do leg crossing and other resistance maneuvers when one gets symptoms in the standing position.
- Begin a graded exercise program under the direction of your physician.
- Drink ample fluid, 48-64 ounces a day often adding solute into the fluid, or taking extra salt up to 6-8 grams a day.
- Drink a bottle of water, 8-16 ounces before even arising in the morning and just dangle the legs over the bed.
- Elevate the head of the bet at night with pillows or with a wedge block. This will avoid a nocturnal diuresis and will prevent one from waking up more dehydrated.
- The patient should wear abdominal binders and compression stockings. We like to start with compression stockings 20-30 mm below the knees and then increase to 30-40 mm if necessary. Oftentimes, we will go waist high and oftentimes we will add an abdominal binder, or use only an abdominal binder if individuals have too much sensitivity to compression and are hypervigilant to compression at the lower extremities.
- An antioxidant cocktail, which should contain Alpha Lipoic Acid at a minimum of 600 mg per day, and prefer up to 1800 mg per day. Also, a nitric oxide-producing compound, which contains beet root extract of at least 500 mg per day is useful in individuals who have significant exercise intolerance with chronic fatigue, or have testing which shows microcirculation abnormalities with nitric oxide production.
If a patient has a stressful lifestyle, stress reduction such as yoga, prayer, or meditation, or Tai-Chi exercises, are extremely important to help relieve Psychosocial stress and the accompanying cellular stress that is depleting her/his antioxidant reserve, depleting the immune systems. Occasionally, they will need some form of pharmacology to reduce stress if there is significant anxiety such as an SSRI.
The good news is that POTS and Orthostatic Intolerance syndromes, especially in young people, are almost never a life-threatening problem and does not lead to major cardiac events. On the other hand, individuals who have Orthostatic Hypotension, or drops in blood pressure, especially individuals over the age of 60, do have higher mortality rates and they need to be tested and assessed more carefully, but this is a topic for another review. POTS should not be diagnosed if a person does have an orthostatic drop in blood pressure, especially more than 20 mm systolic or 10 mm diastolic. Orthostatic drops in blood pressure negate the diagnosis of POTS syndrome.
Pharmacology is usually a temporary feature of treating POTS and many patients may be weaned from the medicines after they undergo an extensive exercise program. Therefore, people with this syndrome complex should be under the care of their physician long-term.



