Click here to download this post
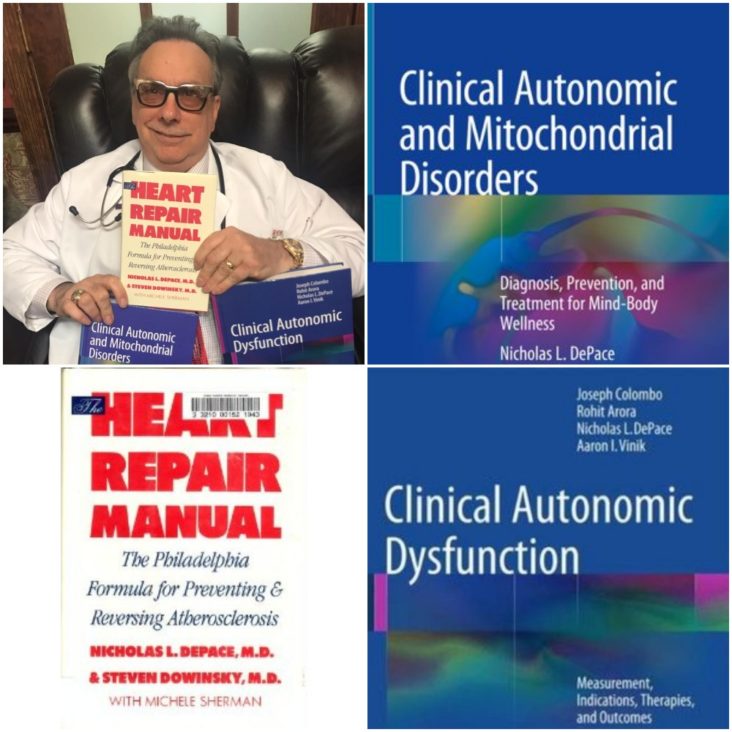
Dr. DePace, MD, FACC
49% of hypermobile EDS (Ehlers-Danlos Syndrome) patients have POTS (postural orthostatic tachycardia syndrome), 31% orthostatic intolerance and 20% have normal hemodynamics. We call this orthostatic intolerance and postural orthostatic intolerance in joint hypermobility syndrome / Ehlers-Danlos hypermobility type, neurovegetative dysregulation or autonomic failure. The autonomic dysregulation is moderate to severe in one-third of our hypermobile EDS patients.
Coat-hanger pain is common in orthostatic intolerance associated with EDS. Coat-hanger syndrome consists of pain at the back of the neck (paracervical) and base of the head (suboccipital) that worsens in the upright position. It is believed to be due to poor blood flow to the muscles of the upper back and neck. It is due to pooling of blood due to abnormal sympathetic nervous system response due to standing and abnormal vasoconstriction. Coat-hanger pain can be quite profound, especially in conjunction with all the other chronic pain seen in EDS patients due to joint hypermobility.
Orthostatic headaches are also seen in EDS due to blood vessel malformation called Chiari malformation, CSF (cerebral spinal fluid) flow issues and CSF leaks. This may collagen problems, leading to stretchy blood vessels in EDS leading to venous pooling. This hypothesis has not been proven; however it makes empiric sense.
Autonomic dysfunction has often been attributed to autoimmunity and many times autoimmune antibodies are not detected, and many believe that this is because they have not been discovered as of yet. Diseases like rheumatoid arthritis, lupus and Sjogren’s disease have been seen with EDS. Nearly 10% had Raynaud’s, which is often associated with autoimmune disorders. It is kissable that abnormalities in the extracellular matrix might contribute to development of autoimmunity in the presence of other genetic or environmental influences.
The most common autoimmune diseases associated with EDS and POTS are Hashimoto’s, Sjogren’s, lupus and celiac disease. However, POTS is not the only dysautonomia disorder that is seen in EDS patients.
Mast cell activation syndrome is often seen in patients who have autonomic dysfunction including POTS and EDS. POTS and mast cell activation syndrome may frequently overlap. POTS patients with EDS tend to report dealing with POTS-like symptoms for most of their life. GI (gastrointestinal) are reported significantly more often by patients with EDS. Sensory neuropathic symptoms have been reported significantly more often in patients with EDS with POTS, including skin burning, hand tingling, hand burning, hand numbness and cold hands. The neuropathy noted in EDS patients suggests that the collagen in and around the nerve fibers may be damaged or abnormal.
Small fiber neuropathy in hypermobile EDS patients likely cause the burning sensations, hypesthesia and allodynia. Small fiber neuropathy refers to dysfunction or damage to the A-Delta and C fibers which relay thermal and nociceptive or unpleasant information as well as mediating autonomic function. There is strong evidence for a peripheral neuropathic contribution to the pain syndrome in hypermobile disorders in addition to the known nociceptive and central sensitization components. This raises the question if there is a neurological cause of hypermobile EDS; the only EDS syndrome without a known genetic cause. Physicians should assess for small fiber pathology in hypermobile EDS patients and hypermobility spectrum disorder patients for sensory and autonomic impact. EDS patients show an overactivity of the resting parasympathetic nerve tone and a decreased sympathetic nerve reactivity to stimuli.