Click Here to Download this Blog Post – Ehlers-Danlos Syndrome (EDS) Prelude – Part 2
By Dr. Nicholas L. DePace, M..D., F.A.C.C – Cardiologist specializing in autonomic dysfunction, Ehlers-Danlos syndrome and POTS.
Overview of Ehlers-Danlos Syndromes (EDS)
Ehlers-Danlos Syndromes (EDS) are a group of 13 heritable connective tissue disorders, which means that you can get it from your parents.
The conditions are caused by genetic changes that affect connective tissue, which is tissue that connects, supports, binds, or separates other tissues or organs. Each type of EDS has its own set of features to identify it.
Core Features Seen Across All EDS Types
Some features are seen across all types of EDS, including joint hypermobility, when joints move beyond their normal range, often due to loose ligaments; skin hyperextensibility, a condition where the skin can be stretched beyond its normal limits because of a problem with the body’s collagen and elastin proteins; and tissue fragility, excessive weakness and susceptibility of tissues to tearing, bruising, and injury.
Hypermobility Spectrum Disorders (HSD)
Patients not meeting strict criteria for EDS may have hypermobility spectrum disorders (HSD) which are connective tissue disorders that cause joint hypermobility, instability, injury and pain.
Additional Symptoms and Related Conditions
Other disorders such as fatigue, a feeling of weariness, tiredness, or lack of energy that can interfere with daily life; headaches, GI problems, a wide range of conditions affecting the digestive tract, with symptoms like abdominal pain, bloating, heartburn, nausea, and changes in bowel habits; and autonomic dysfunctions, a condition where the autonomic nervous system, which controls automatic bodily functions like heart rate, blood pressure, and digestion, doesn’t work properly are often seen as part of EDS/HSD [Ehlers Danlos Society].
Understanding Autonomic Dysfunction in EDS/HSD
Symptoms of EDS and hypermobility may be traced to the parasympathetic, a division of the autonomic nervous system that promotes “rest and digest” functions, counteracting the “fight or flight” response of the sympathetic nervous system; and sympathetic nervous system, a part of the autonomic nervous system that triggers the body’s “fight-or-flight” response to stress or danger; or oxidative stress, an imbalance between the production of free radicals and the body’s ability to detoxify them through antioxidants, leading to cellular damage; and all are treatable.
Clinical Approach to EDS & HSD
As a practicing Clinical Internist, I am always prepared to diagnose a patient with numerous “somatic complaints”, physical symptoms, like pain, fatigue, or dizziness, that cause significant distress or interfere with daily life, with a syndrome rather than to attribute them as psychosomatic, physical symptoms caused by mental factors like stress, anxiety, or emotional disturbance, which is always easier to do and which the majority of physicians prior to a patient’s visit with me have done. Such applies to patients who present with undiagnosed Ehlers-Danlos Syndrome (EDS) or Hypermobility Spectrum Disorder (HSD).
Why Expert Evaluation Matters
It is important to seek out a clinician with expertise in EDS to make an accurate diagnosis and create a treatment plan. One of the nation’s leading centers is Franklin Cardiovascular Associates, under the direction of Nicholas DePace, MD, FACC. They are located in Sicklerville, New Jersey. franklincardiovascular.com, (856) 589-6034
About the Author
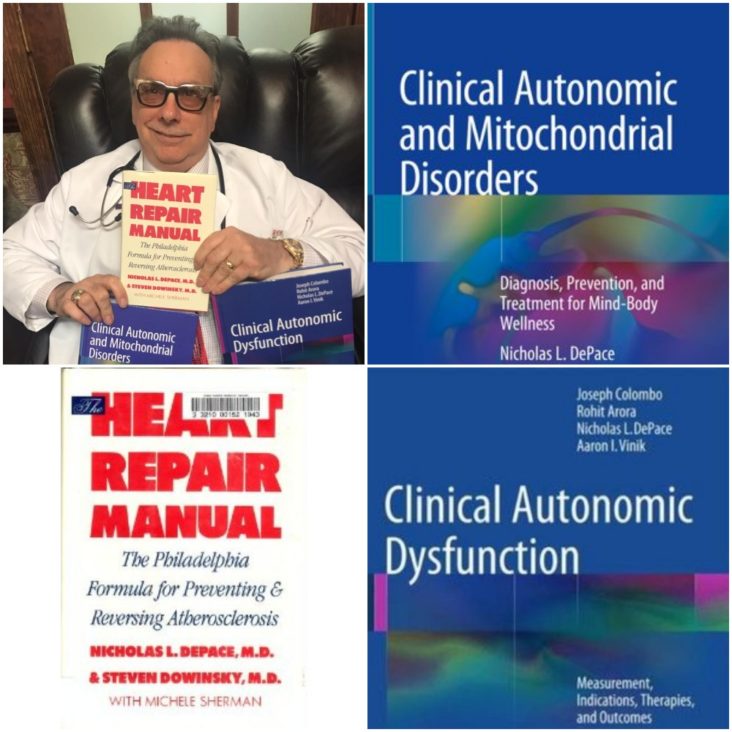
Nicholas L. DePace, MD, FACC is a board-certified cardiologist and Medical Director of Franklin Cardiovascular Associates. A graduate of the Mount Sinai School of Medicine, Dr. DePace has decades of clinical, academic, and research experience and has held faculty appointments as a Clinical Professor of Medicine, becoming one of the youngest full professors in Philadelphia at the time of his appointment.
Dr. DePace specializes in the diagnosis and treatment of autonomic nervous system dysfunction (dysautonomia), including POTS, autonomic dysfunction associated with Ehlers-Danlos syndrome (EDS), chronic fatigue, and anxiety-like conditions that are frequently misdiagnosed. He is nationally recognized for his work on parasympathetic and sympathetic (P&S) nervous system imbalance, a core mechanism underlying many complex chronic disorders.
In addition to treating patients from across the United States, Dr. DePace is a prolific clinical researcher and author of multiple nationally distributed medical textbooks published by Springer and W.W. Norton, focusing on autonomic dysfunction, mitochondrial disorders, cardiovascular disease, and mind–body medicine.
👉 View Dr. DePace’s professional profile
👉 View medical books by Dr. DePace