Click Here to Download this Blog Post – The Invisible “Wiring” Problem (Part 12)
By Dr. Nicholas L. DePace, M..D., F.A.C.C – Cardiologist specializing in autonomic dysfunction, Ehlers-Danlos syndrome and POTS.
What Is Autonomic Dysfunction in hEDS?
If you live with Hypermobile Ehlers-Danlos Syndrome (hEDS) or Hypermobility Spectrum Disorder (HSD), you might feel like your body is constantly playing tricks on you. One minute you’re fine, and the next, simply standing up makes you feel dizzy, foggy, or anxious.
You aren’t imagining it, and it isn’t “just stress.”
For the vast majority of people with connective tissue disorders, the root cause of these mysterious symptoms isn’t a problem with your heart or your brain structure—it’s a glitch in your body’s “autopilot,” formally known as the Autonomic Nervous System.
Here is a breakdown of what is happening inside your body, translated from medical jargon into plain English.
How the Autonomic Nervous System Works (Gas vs Brake)
To understand the glitch, we first have to look at how the system should work. Your autonomic nervous system controls the things you don’t have to think about, like heart rate and digestion. It has two main modes:
- The Sympathetic System (The Gas Pedal): This is your “fight or flight” mode. It speeds you up and tightens your blood vessels to pump blood to your brain when you stand up or face stress.
- The Parasympathetic System (The Brake Pedal): This is your “rest and digest” mode. It slows your heart down and helps you relax and eat.
In a typical body, these two work in perfect harmony. In hEDS/HSD patients, they often get confused.
The Two Nervous System Glitches in hEDS
Research shows that most patients with these connective tissue disorders struggle with two specific “wiring” issues:
-
The Brake Gets Stuck (Parasympathetic Excess)
Imagine you are driving and suddenly encounter a stressful situation. You need to react, but instead of the car accelerating, the brake pedal gets slammed down. This is Parasympathetic Excess. When you face stress, your body reacts with too much “calming” signal, which can paradoxically make you feel worse.
-
The Gas Pedal Fails (Sympathetic Withdrawal)
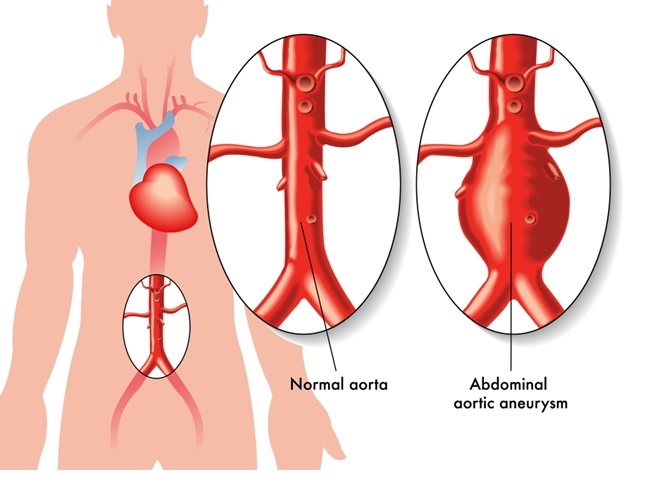
This is the big one for daily life. When you stand up, gravity naturally pulls your blood down into your legs. A normal body immediately hits the gas (Sympathetic system) to tighten blood vessels and push that blood back up to your brain.
In many hEDS/HSD patients, this doesn’t happen. The “gas pedal” fails to engage. The blood vessels stay loose, and gravity wins.
Blood Pooling in hEDS: Why Standing Makes You Feel Worse
Because of Sympathetic Withdrawal, when you are upright, blood pools in your legs rather than flowing up to your vital organs. This leads to poor perfusion (a fancy word for “not enough blood flow”).
When your brain and heart don’t get the fuel they need, you experience:
- Brain Fog: Your brain is literally running on low battery.
- Fatigue & Fainting: Your body is exhausted from trying to fight gravity.
- Digestion Issues: Your stomach and intestines rely on these nerves to move food along. When the nerves misfire, you get bloating, nausea, or irregular bathroom habits.
Why hEDS Symptoms Mimic Anxiety Disorders?
One of the most frustrating parts of this condition is being told it’s “all in your head.”
When your brain isn’t getting enough oxygen-rich blood, it panics. This physical lack of blood flow can trigger symptoms that look exactly like:
- Anxiety and Depression
- ADHD (trouble focusing)
- Panic attacks
- Bipolar disorder
Furthermore, because your heart is starving for blood, it might race or pound (palpitations) to try to compensate. This often leads to scary trips to the ER for “chest pain” or “shortness of breath,” only to be told your heart is perfectly healthy.
And that’s the key: Your organs (the hardware) are usually fine. It is the nerves controlling them (the software) that are lagging.
How Autonomic Dysfunction in hEDS Is Diagnosed and Treated?
Understanding this mechanism is half the battle. This is not a structural defect in your heart or a psychiatric breakdown; it is a physiologic mismatch.
The path forward involves:
- Proper Testing: Doctors can test your “P&S” (Parasympathetic and Sympathetic) nerves to prove the organs are healthy but the signals are crossed.
- Reassurance: Knowing your heart isn’t failing can reduce the fear associated with the symptoms.
- Treatment: Unlike structural heart defects, nerve signaling can often be managed and retrained with the right medication and lifestyle changes tailored to your specific “wiring.”
You aren’t broken; your autopilot just needs a reset.
Where to Seek Expert Care?
It is important to seek out a clinician with expertise in EDS to make an accurate diagnosis and create a treatment plan. One of the nation’s leading centers is Franklin Cardiovascular Associates, under the direction of Nicholas DePace, MD, FACC. They are located in Sicklerville, New Jersey. franklincardiovascular.com, (856) 589-6034
About the Author
Nicholas L. DePace, MD, FACC is a board-certified cardiologist and Medical Director of Franklin Cardiovascular Associates. A graduate of the Mount Sinai School of Medicine, Dr. DePace has decades of clinical, academic, and research experience and has held faculty appointments as a Clinical Professor of Medicine, becoming one of the youngest full professors in Philadelphia at the time of his appointment.
Dr. DePace specializes in the diagnosis and treatment of autonomic nervous system dysfunction (dysautonomia), including POTS, autonomic dysfunction associated with Ehlers-Danlos syndrome (EDS), chronic fatigue, and anxiety-like conditions that are frequently misdiagnosed. He is nationally recognized for his work on parasympathetic and sympathetic (P&S) nervous system imbalance, a core mechanism underlying many complex chronic disorders.
In addition to treating patients from across the United States, Dr. DePace is a prolific clinical researcher and author of multiple nationally distributed medical textbooks published by Springer and W.W. Norton, focusing on autonomic dysfunction, mitochondrial disorders, cardiovascular disease, and mind–body medicine.
👉 View Dr. DePace’s professional profile
👉 View medical books by Dr. DePace