Click Here to Download this Blog Post – It’s Not “All in Your Head”—It’s Lack of Blood Flow to Your Head (Part 10)
By Dr. Nicholas L. DePace, M..D., F.A.C.C – Cardiologist specializing in autonomic dysfunction, Ehlers-Danlos syndrome and POTS.
How hEDS and HSD Symptoms Connect to the P&S Nervous System
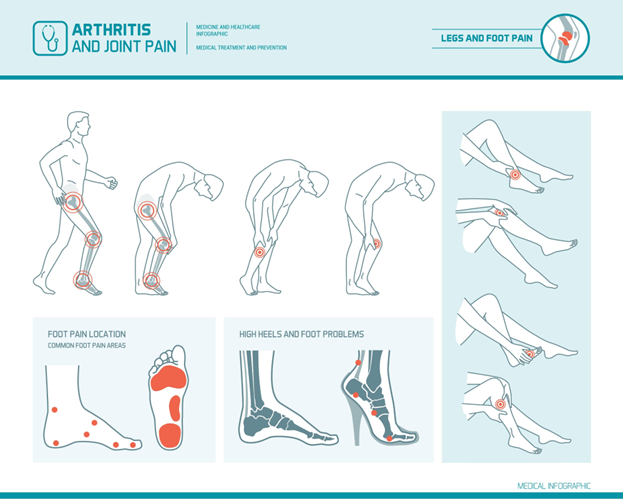
If you have hEDS (Hypermobile Ehlers-Danlos Syndrome) or HSD (Hypermobility Spectrum Disorder), you are likely used to dealing with pain and loose joints. But for many patients, the symptoms that actually disrupt daily life the most—brain fog, anxiety, racing hearts, and stomach issues—seem completely unrelated to their joints.
The truth is, they are directly connected through your P&S Nervous System (Parasympathetic and Sympathetic systems).
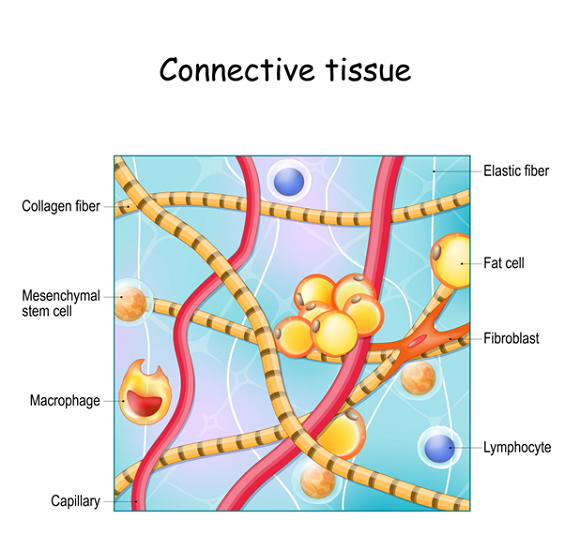
When you have hEDS, your “hardware” (your heart, brain, and stomach organs) is usually perfectly healthy. The problem is the “software” (the nerves telling them what to do) is glitching. Here is how that glitch works.
The Two Main Glitches in hEDS and HSD
Most hEDS patients suffer from two specific types of nervous system dysfunction:
-
Sympathetic Withdrawal (The “Failure to Squeeze”)
Normally, when you stand up, your Sympathetic nerves (fight or flight) tell your blood vessels to squeeze tight to push blood up against gravity. In hEDS patients, these nerves often fail to react—we call this Sympathetic Withdrawal.
- The Result: Gravity wins. Blood pools in your legs.
- The Consequence: Your heart, brain, and arms don’t get enough blood flow. This leads to profound fatigue, fainting, and cold hands.
-
Parasympathetic Excess (The “Over-Reaction”)
Your Parasympathetic system is supposed to be your “Rest and Digest” mode. However, in hEDS patients, this system often overreacts to stress.
- The Result: Instead of calming you down, it amplifies pain signals and disrupts your digestion.
- The Consequence: This leads to GI issues (stomach paralysis or urgency), bladder issues, and a heightened sensitivity to pain.
The “Great Masquerader”: Why It Looks Like Anxiety or Heart Disease
Because of Sympathetic Withdrawal, your brain and heart are constantly starved of the blood flow they need to function optimally. This leads to symptoms that mimic other serious diseases, leading to misdiagnoses.
The “Heart Attack” Mimic
When your heart isn’t getting enough blood flow because it’s pooling in your legs, it races and pounds to try to compensate.
- Symptoms: Chest pain, palpitations, shortness of breath.
- The Reality: Patients are often terrified they have heart disease, but the heart muscle is healthy. It’s just working overtime because of the blood flow issue.
The “Mental Health” Mimic
When the brain doesn’t get enough blood flow (poor cerebral perfusion), it starts misfiring. This is perhaps the most validating discovery for many patients.
- Symptoms: Brain fog, inability to focus, mood swings, and panic.
- The Misdiagnosis: These symptoms often look exactly like Anxiety, Depression, Bipolar Disorder, OCD, or ADD/ADHD.
- The Reality: While these conditions can coexist, often the “anxiety” or “attention deficit” is actually the brain panicking because it isn’t getting enough oxygen and fuel. Even unexplained seizures can sometimes be traced back to this lack of blood flow.
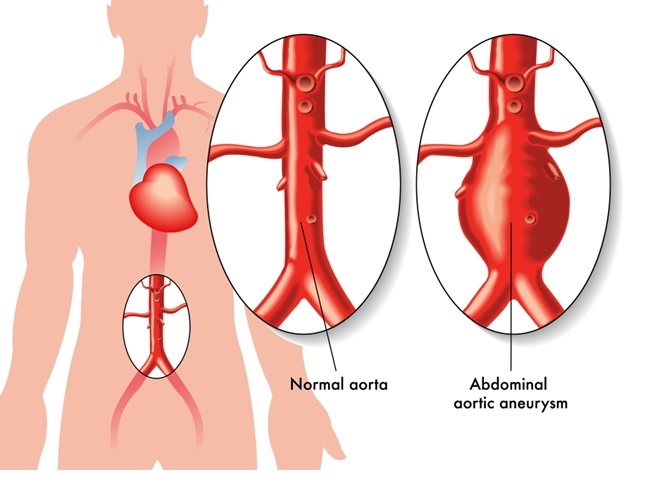
A Note on Safety: The Vascular EDS Distinction
While we focus heavily on the quality of life for hEDS patients, we must always keep an eye out for Vascular EDS (vEDS).
As mentioned in previous posts, vEDS is the rare, life-threatening form. Unlike the “bendy” hEDS patients who faint and hurt, vEDS patients are defined by tissue fragility.
- The Clue: If a patient (especially under 40) has a history of organ rupture (like intestines), aneurysm, or severe bleeding that goes beyond simple bruising, we must suspect vEDS.
- The Distinction: hEDS is about pain and dizziness. vEDS is about tissue fragility and bleeding.
The Path Forward for hEDS/HSD Patients
The most important takeaway is this: Your organs are likely healthy.
The treatment for hEDS/HSD isn’t about fixing a “broken” heart or a “broken” brain. It is about fixing the P&S nerve signals. Through proper testing, we can prove that your organs are fine, which is reassuring!
Once we know it’s a “software” issue, we can create a personalized plan to help your nerves communicate better, keeping your blood where it belongs: in your head and heart.
Where to Seek Expert Care
It is important to seek out a clinician with expertise in EDS to make an accurate diagnosis and create a treatment plan. One of the nation’s leading centers is Franklin Cardiovascular Associates, under the direction of Nicholas DePace, MD, FACC. They are located in Sicklerville, New Jersey. franklincardiovascular.com, (856) 589-6034
About the Author
Nicholas L. DePace, MD, FACC is a board-certified cardiologist and Medical Director of Franklin Cardiovascular Associates. A graduate of the Mount Sinai School of Medicine, Dr. DePace has decades of clinical, academic, and research experience and has held faculty appointments as a Clinical Professor of Medicine, becoming one of the youngest full professors in Philadelphia at the time of his appointment.
Dr. DePace specializes in the diagnosis and treatment of autonomic nervous system dysfunction (dysautonomia), including POTS, autonomic dysfunction associated with Ehlers-Danlos syndrome (EDS), chronic fatigue, and anxiety-like conditions that are frequently misdiagnosed. He is nationally recognized for his work on parasympathetic and sympathetic (P&S) nervous system imbalance, a core mechanism underlying many complex chronic disorders.
In addition to treating patients from across the United States, Dr. DePace is a prolific clinical researcher and author of multiple nationally distributed medical textbooks published by Springer and W.W. Norton, focusing on autonomic dysfunction, mitochondrial disorders, cardiovascular disease, and mind–body medicine.
👉 View Dr. DePace’s professional profile
👉 View medical books by Dr. DePace