Click Here to Download this Blog Post – The Invisible Condition (Part 6)
By Dr. Nicholas L. DePace, M..D., F.A.C.C – Cardiologist specializing in autonomic dysfunction, Ehlers-Danlos syndrome and POTS.
What Makes hEDS and HSD “Invisible Conditions”?
Hypermobile Ehlers-Danlos Syndrome (hEDS) and Hypermobility Spectrum Disorders (HSD) are conditions that often go unnoticed (“invisible”) for decades because they are difficult for doctors to spot.
Key Takeaways in Simple Terms
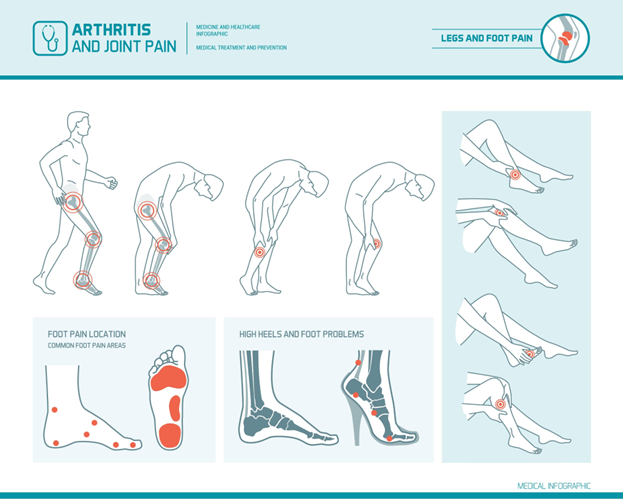
- What are Hypermobile Ehlers-Danlos Syndrome (hEDS) and Hypermobility Spectrum Disorders (HSD)? hEDS and HSD are very similar conditions where the joints are too flexible (hypermobile) and unstable. While they used to have different names, they both result in the same problems: loose joints, muscle pain, frequent injuries, and eventually arthritis. Doctors diagnose this by checking how flexible you are using a checklist called the Beighton Criteria.
- The Main Symptom: Chronic Pain The biggest complaint from patients is widespread, long-lasting pain.
- When does it start? For most people (75%), pain starts in their teenage years. However, for some, it doesn’t start until they are in their 50s or 60s.
- Why does it hurt? The pain is usually linked to how unstable the joints are. The looser the joints, the worse the pain tends to be.
- Exhaustion and Poor Sleep Patients are often constantly tired. This isn’t just laziness; it is caused by:
- Nervous system issues (P&S dysfunction).
- Physical disruption: Joints can actually slip out of place (sublux) just by rolling over in bed, ruining sleep quality.
- The Cycle of Misdiagnosis Because the condition “hides,” patients are frequently misdiagnosed before doctors realize they have loose joints. Common wrong diagnoses include:
- Chronic Fatigue Syndrome
- Fibromyalgia
- Depression
- Hypochondriasis (being told “it’s all in your head”)
- Malingering (being accused of faking it)
Conclusion Over the last 30 years, experts have realized that this is not just a joint problem. It is a whole-body condition that affects many different systems, causing significant suffering that often goes untreated for years.
It is important to seek out a clinician with expertise in EDS to make an accurate diagnosis and create a treatment plan. One of the nation’s leading centers is Franklin Cardiovascular Associates, under the direction of Nicholas DePace, MD, FACC. They are located in Sicklerville, New Jersey. franklincardiovascular.com, (856) 589-6034