Click here to download this post
COVID-19 Prevention Tips: Exercise And Nutrition
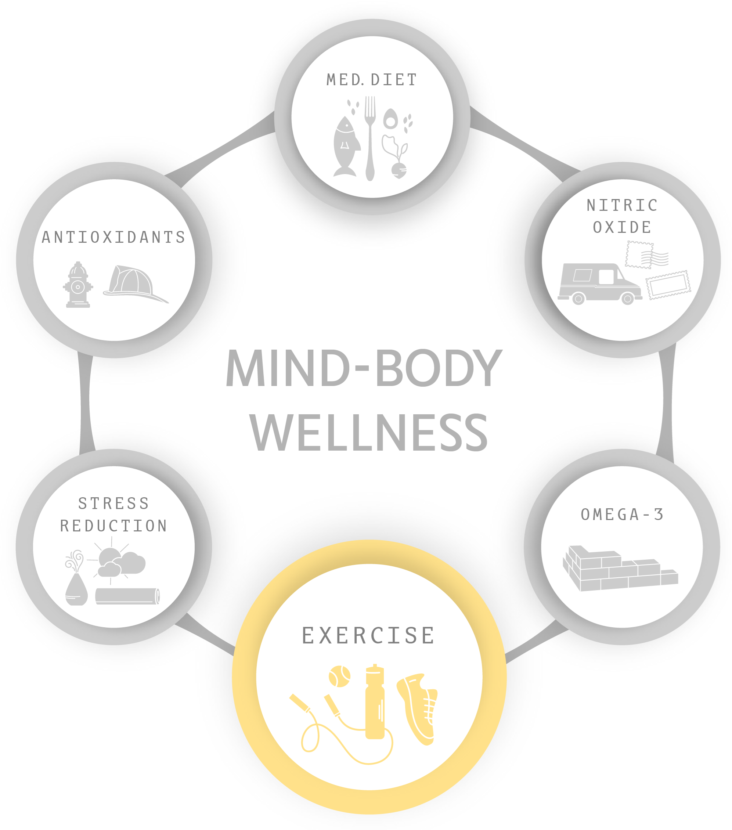
COVID-19, the Coronavirus, like the flu (e.g., the Influenza virus) and similar to colds, may be prevented or mitigated, and are often treated, by the combination of a healthy diet and exercise, and perhaps additional antioxidant; the most common being Vitamin C in some form: fresh, ripe fruits and vegetables are preferable, and supplements are also good.
In fact, many typically healthy people have contracted COVID-19 and have recovered. Many more have contracted it and may have even had mild symptoms, but never knew they had it until after having recovered from COVID-19. This is similar to cases with the Influenza virus or the flu. So like, the flu, those at risk need to protect themselves and take necessary precautions to stay healthy. Again, the major contribution to health, even if you are at risk, is a healthy diet full of fresh fruits and vegetables and exercise.
EXERCISE
 Please, EXERCISE IS NOT A DIRTY WORD! It does not have to be drudgery. We are not talking about going to the gym and beating yourself up for hours. Perhaps a better description is “ACTIVE LIFESTYLE,” which may include exercise (in the sense of the current vernacular), but it should reflect the lifestyle of people before automobiles, elevators, television remotes, and cell phones. It can be a single (preferably daily) acute bout of physical exertion or muscular activity that expends energy above one’s basal or resting level – frequent movement of some sort. It is true, siting has become the “new smoking.” For those who are old enough, we are referring to a time before electronics, when play was not sitting around with computer games getting strong thumbs and weak bodies and communicating with someone was not done electronically developing stronger thumbs. People walked places or rode their bikes, children were outside walking, skipping, running, jumping, breathing fresh air and soaking in sunshine for their daily dose of Vitamin D. Adults would do house work, garden, yard-work, walk to the corner store, walk over to the neighbors to check on the children, or have a cup of coffee or tea and catch up on the news of the neighborhood, or simply play with the children at home, take the stairs or shop, etc. Life was not sedentary. Life included what we mean by exercise.
Please, EXERCISE IS NOT A DIRTY WORD! It does not have to be drudgery. We are not talking about going to the gym and beating yourself up for hours. Perhaps a better description is “ACTIVE LIFESTYLE,” which may include exercise (in the sense of the current vernacular), but it should reflect the lifestyle of people before automobiles, elevators, television remotes, and cell phones. It can be a single (preferably daily) acute bout of physical exertion or muscular activity that expends energy above one’s basal or resting level – frequent movement of some sort. It is true, siting has become the “new smoking.” For those who are old enough, we are referring to a time before electronics, when play was not sitting around with computer games getting strong thumbs and weak bodies and communicating with someone was not done electronically developing stronger thumbs. People walked places or rode their bikes, children were outside walking, skipping, running, jumping, breathing fresh air and soaking in sunshine for their daily dose of Vitamin D. Adults would do house work, garden, yard-work, walk to the corner store, walk over to the neighbors to check on the children, or have a cup of coffee or tea and catch up on the news of the neighborhood, or simply play with the children at home, take the stairs or shop, etc. Life was not sedentary. Life included what we mean by exercise.
The physiologic and psychologic benefits of exercise are numerous. It is better than any supplement or pill available, and what we mean by exercise is infinitely less expensive. Again, it is probably better than any combination of supplements or pills or possibly even pharmacological agents available. In fact, exercise with supplements, etc., including diet which supports exercise, is the best combination for minimizing the risk of illness, including flu conditions, like COVID-19. Exercise optimizes quality and continuation of life, and minimizes mortality risk, which optimizes longevity and minimizes the impact of disease if and when it happens. While the diet fuels exercise and provides the nutrients needed for good health, exercise provides many health benefits, like simulated fever and being (arguably) the strongest antioxidant available. The list of benefits includes:
Wards-off Viruses and other pathogens trying to invade your body by simulating fever. Exercise raises your core body temperature. Most pathogens are killed by elevated temperatures (like above 101°F). Our recommended 40 minute walk at 2 mph typically reaches this core body temperature goal and helps to prevent viruses and other pathogens from gaining a foothold in your body. In effect the higher temperatures help to “burn-out” the invaders, including viruses.
Happier Moods from the release of endorphins in the brain, and other brain chemicals that elevate mood. Regular physical activity (3 to 5 times a week for 30 to 60 minutes each time) reduces risk of depression.
Immune Health from two aspects of exercise as mentioned above: 1) Exercise (physical activity) raises the body’s core temperature, simulating a  fever (20 minutes or more of exercise, three or more times per week helps to prevent disease before is starts); 2) Exercise is arguably the strongest antioxidant available and provides all of the benefits of antioxidants (like Vitamin C), including defeating (promoting the oxidation of) all types of infections: viral, bacterial, fungal, etc.
fever (20 minutes or more of exercise, three or more times per week helps to prevent disease before is starts); 2) Exercise is arguably the strongest antioxidant available and provides all of the benefits of antioxidants (like Vitamin C), including defeating (promoting the oxidation of) all types of infections: viral, bacterial, fungal, etc.
Reduced Pain. Endorphins are natural pain killers and can help to provide temporary pain relief.
(The brief explanations of the rest of these benefits are available at the end of this document.)
Better Sleep Quality.[1]
Improved Concentration & Creativity.[2]
Reduce Stress Levels & Anxiety.[3]
Maintain Mental Fitness.[4]
Parasympathetic and Sympathetic (P&S) Nervous Systems.[5]
Stress Reduction.[6]
Heart & Vascular Health.[7]
Neuroendocrine Health.[8]
Weight Control (Loss).[9]
Reduced Risk of Type 2 Diabetes and Metabolic Syndrome.[10]
Reduced Cancer Risk.[11]
Strengthen Bones and Muscles.[12]
Promotes Longevity (promotes living longer).[13]
CAUTION: As always, an exercise regimen should be started under close physician supervision. The wrong types of exercise may do more harm than good, including increasing body fat (and thereby weight), fatigue, and pain due to the fact that the body is programmed to over-react to stresses. Under these conditions, the body sees exercise as stress and works to protect itself against the stress. With certain diseases (e.g., some arrhythmias, diabetes, stroke or aneurysm risk, or heart disease), the wrong type of exercise may also lead to heart attack, stroke, or sudden death. It is best to start slow and build up and always listen to your body. Until endurance built, recommended goals may not be reached for a while. This is not bad; keep at it until the goals are reached. The health benefits of physical activity far outweigh the risks of getting hurt.
As with a pure Mediterranean diet, strict compliance with the recommended 150 minutes of exercise per week is not required to get beneficial effects. Smaller amounts of exercise are helpful, just not as much.
ANTIOXIDANTS
Again, exercise is the strongest antioxidant possible. Less than healthy people, especially those at most risk, because of age or illness have fewer naturally available antioxidants made by their bodies. Either (1) aging slows the production or (2) the disease is causing the immune system to use them faster than normal and out-pacing the body’s production. Alpha-Lipoic Acid (ALA, specifically (r)ALA*) and CoQ10 are arguably the two most powerful antioxidants your body makes, and they are made more powerful by the fact that they recycle other antioxidants (like Vitamin C, as well as Vitamins A & E, and Glutathione). The fact that (1) exercise is arguably the most powerful antioxidant of all and (2) healthy youngsters are more active (exercise more) and are making more ALA and CoQ10 naturally than older or sicker folks, goes a long way to explaining the difference in the reaction of healthy youngsters versus healthy older folks. It also explains why the more active older folks we know that have contracted COVID-19 have all survived.
In addition to helping the immune system, antioxidants also help keep Mitochondria healthy, especially ALA (in the nerves) and CoQ10 in the heart muscle. Again, exercise enhances this as well, as well as releases the endorphins, which helps to minimize depression and anxiety. By elevating mood, illness is minimized or prevented. The cascade goes on. There is a lot of this in the second book we wrote.[14]
IMMNUNE RESPONSES
Some doctors and scientists are reporting that an immune system gone haywire may be doing more damage than the coronavirus itself in patients with the severest forms of COVID-19. Exercise, Antioxidants and a proper diet help to stabilize the immune system and keep it stable. In the case of Severe Acute Respiratory (SAR) type viruses, the out-of-control immune response eventually causes the patients’ lungs to stop delivering oxygen to the body leading to respiratory failure. It may also cause excessive inflammation that adds to fluid generation in the lungs. It may also weaken blood vessels adding more fluid in the lungs further exacerbating respiratory failure and, in some cases, may cause death. In this way, the malfunctioning (overactive) immune system may be driving the rapid decline in lung function experienced by some patients.
We have found that the immune system is controlled and coordinated by the Parasympathetic Nervous System. Further, we have found that an over-active immune system is associated with an over-active Parasympathetic Nervous System, and the opposite is true as well. We have labeled an over-active Parasympathetic Nervous System as Parasympathetic Excess, or PE. For example, brain trauma patients with PE are found to have a higher incidence of life threatening pneumonia than those brain trauma patient s without PE. We have also found that normalizing PE helps to stabilize the immune system and reduces mortality and morbidity risk.
[*] There are two isomers of Alpha-Lipoic Acid, (r) and (s). Only (r) is used by the body. The (s) isomer is used for filler and less expensive products.
To slow or stop this process, some are being prescribed standard courses of anti-inflammatories, including steroids, including high dose steroids. Some believe, high dose steroid is also accepted treatment for COVID-19, therefore if administered prior to detection of COVID-19 may mask COVID-19 in these patients until late in the progression of the disease. Excessive amounts of steroids may also suppress the immune system which of course would have a negative effect. Having experienced this, we strongly recommend that patients on high dose steroids be screen for COVID-19, as a precaution.
ANGIOTENSIN RECEPTORS
In a similar vein, evidence suggests that COVID-19 gains entry into cells through the ACE2 receptor. ACE stands for Angiotensin Converting Enzyme. ACE-Inhibitors (ACE-Is) and Angiotensin Receptor Blockers (ARBs) are commonly prescribed to patients with high blood pressure (Cardiovascular disease patients and patients with Diabetes). Of course, the connection has caused concern within these communities. However, the Cardiology communities (ACC & AHA) have stated that ACE-Is and ARBs are still considered safe and, perhaps, without these medications, those patients would be more at risk for infection (COVID-19 or other). The concern is that by taking ACE-Is or ARBs, the number of ACE2 receptors in the body will increase, which they will, and that this increase may provide more entry points for the virus. However, the latter is not likely. In Angiotensin-mediated Hypertension (HTN), the number of ACE2 receptors is already elevated. That had already contributed to the HTN. ACE-Is and ARBs are designed to block the excess receptors to begin with and even block some of the original receptors to ensure lower blood pressure. If these receptors are already blocked to limit their use for raising blood pressure, then it is not likely that COVID-19 will be able to use them either. Think of a lock and a key. Once a key is inserted into the lock, another key cannot be inserted. The ACE-I or ARB is the first key. COVID-19 is the second key and is also blocked.
While ACE-Is and ARBs may help those patients to whom they are prescribed have lower risk to COVID-19, they are not being recommended for patients who do not qualify under the guidelines for those medications. Remember, the patients who are prescribed ACE-Is and ARBs were already at risk due to the HTN. If you are already prescribed an ACE-I or ARB do not stop it. If you are not already prescribed an ACE-I or ARB do not start it without physician permission. As always, never take medication without consulting your physician first.
OXIDATIVE STRESS
There is another aspect to the Coronavirus (COVID-19). The Coronavirus like other viruses and significant infections cause oxidative stress. Oxidative stress is a stress to the cells of your body. It is the result of something, in this case COVID-19, attacking the cells’ energy production processes. The primary component (organelle) responsible for energy production is the Mitochondria. Mitochondria are like power plants in many ways. They produce energy. They also produce waste. However, in the case of cells, the waste is not considered pollution, it is actually used, and under healthy conditions, all of it used; nothing is wasted.
The waste products are oxidants. Yes, the very things that destroy cells, and we try to flood our systems with their opposites – antioxidants – are the very things that the Mitochondria make as waste products. Again, under healthy conditions these oxidants are not “pollutants.” They are used by a healthy immune system to “burn the trash.” Pathogens (things invading our bodies and trying to make us sick) enter our bodies every moment. As long as we are in familiar places, our bodies already have developed a defense mechanism against all of these pathogens, and in addition to fever, another first line of defense is to use the oxidants to burn the trash. However, once the trash pile is burned, the fire must be extinguished. The antioxidants are the fire extinguishers, or buckets of water if you will, to put out the fire before it burns healthy tissue. Therefore, a small amount of oxidant production is healthy, as long as there is an ample supply of antioxidant on hand as well.
Again, as we age or are ill for long periods of time, the natural production of antioxidants declines, and again, fortunately, they may be supplemented. However, if they are not supplemented sufficiently, the virus may leave behind oxidative stress. Unfortunately, oxidative stress only reduces the functioning of cells. This is unfortunate because the organs remain largely functional, and structurally, remain within normal limits. Therefore, at rest (which is when most doctors assess their patients – sitting or lying down), these patients seem normal. Yet they complain of fatigue (sometimes debilitating fatigue), lightheadedness or dizziness, poor sleep, brain-fog, memory and cognitive difficulties, sex dysfunction, GI upset (both upper and lower), sensory and temperature hypersensitivity, headache or migraine, depression or anxiety, generalized pain, and more. While it is difficult to measure oxidative stress, we are now able to directly measure its effects, especially on the Parasympathetic and Sympathetic (P&S) nervous systems.
P&S Monitoring helps to document the effects of any serious illness, including oxidative stress due to viruses, including COVID-19, which may leave significant oxidative stress behind. Since oxidative stress does not do overt damage to the organ system, affecting primarily the mitochondria, cells’ function is sub-par, these patients are affected when they attempt to be active. It is like having a clogged fuel filter on your car. Your car will start and idle just fine, but as soon as you hit the gas the engine begins to choke and you are unable to move or move very fast. Oxidative stress primarily affects the Parasympathetic nervous system, causing it to be more active. If the Parasympathetics are already overactive (PE) due to immune system excesses, this additional Parasympathetic activation only serves to exacerbate the whole problem and these patients rapidly deteriorate into disability claims, yet they appear healthy. With no specific disorder, unless the P&S nervous systems are measured independently and simultaneously (as only the technology that we have can – P&S Monitoring), patients will go from doctor to doctor for years and perhaps decades, including recommendations for psychological evaluation, before they find someone with P&S Monitoring, if ever. In the meantime, they are disabled, out of work, have very poor qualities of life, and are at higher risk for infections such as COVID-19.
CASE IN POINT
A recent patient was admitted to hospital with Inflammatory Myopathy, a large group of potentially treatable myopathies in both children and adults [15]. They represent a heterogeneous group of disorders which include the Dermatomyositis, Polymyositis, Immune-Mediated Necrotizing Myopathy (IMNM), and Inclusion Body Myositis. There are various strategies for treating Inflammatory Myopathies especially IMNM. IMNM accounts for approximately one-fifth of all Inflammatory Myopathies and present with severe muscle weakness and high creatinine levels. They are often seen after viral infections, malignancies (cancer) or connective tissue disorder such as Rheumatoid Arthritis, Lupus and Scleroderma, but can be seen in patients taking statins.
Many of these patients have resistance to conventional immunosuppressive therapy [16]. IMNM is distinguished by the absence of primary inflammation on muscle biopsy and may be associated with myositis-specific autoantibodies. Prompt treatment is important especially in patients who develop acute or progressive swallowing or breathing abnormalities from difficulty with skeletal muscle function. Prednisone is first-line treatment, but is oftentimes ineffective and second-line treatment needs to be employed. Second-line treatment may include disease-modifying agents, such as Methotrexate, Azathioprine or Mycophenolate Mofetil. Additional second-line treatment includes Intravenous Immunoglobulin (IVIG). Recent research has suggested a high rate of response to Rituximab in patients with autoimmune myopathies [17].
Immunosuppressive therapy increases the risk of infection including Aspiration Pneumonia [17,18]. Pneumococcal vaccine and yearly Influenza vaccinations are recommended. Before starting second-line treatment, it has also been recommended to screen for Tuberculosis and Hepatitis B and C. There are no consensus guidelines for Pneumocystis Pneumonia (PCP).
With the emergence and spread of the 2019 novel Coronavirus (COVID-19) it has become imperative to consider this virus when beginning patients on immunosuppressive therapies. The virus originated in bats and was transmitted to humans through unknown intermediary animals in Wuhan-Hubei Province, China, in December 2019. Patients present with fever, cough, sore throat, breathlessness, fatigue, malaise and other symptoms. This is predominately an upper respiratory infection. However, a large subset of patients may be asymptomatic [19]. In February 2020, the World Health Organization (WHO) designated the disease COVID-19, which stands for Coronavirus Disease 2019 [20]. The virus that caused COVID-19 is designated as Severe Acute Respiratory Syndrome Coronavirus 2(SARS-CoV-2).
This was a case of acute relapsing, remitting IMNM, with progressive severe life-threatening Dysphagia that required enteral feeding and aggressive immunosuppressive treatment. The patient had no significant symptoms consistent with acute Coronavirus infection and underwent first IVIG treatment, Mycophenolate Mofetil, and subsequently plasma exchange treatment. After just beginning plasma exchange treatment the patient became acutely Hypoxemic and Hypotensive and sustained a fatal cardiorespiratory arrest. Postmortem reporting of respiratory secretions at the time of the cardiac arrest disclosed what was positive for COVID-19. We now propose that even in asymptomatic rheumatological patients with rheumatological disease who are starting advanced immunosuppressive therapy that they be screened for COVID-19 in addition to Tuberculosis and viral Hepatitis.
This is an unfortunate case of a patient with a five-year history of IMNM who, on presentation, initially responded to IVIG, but with the most recent acute flare-up did not have a good response. Despite high-dose intravenous steroids, IVIG, Mycophenolate (CellCept) and subsequent plasma exchange, the patient did not respond and had an acute deterioration with Hypoxemia, Hypotension, and Cardiorespiratory Arrest, all of which occurred suddenly. Microbiology disclosed COVID-19. Pre-mortem, prior to the patient’s Cardiopulmonary arrest, this infection was not suspected. He had no fever or salient cough. His shortness of breath appeared to be related to volume overload due to diastolic dysfunction, which responded to diuretics. He had no significant radiographic infiltrates and no signs of elevated inflammatory markers. The patient was, however, on high-dose steroids which may have suppressed fever and an inflammatory response.
Among subsets of patients at high risk of developing severe infections are patients with Rheumatic diseases including Lupus, Rheumatoid Arthritis, Scleroderma, Inflammatory Myopathies, and Vasculitis [17, 21]. The European League Against Rheumatism released guidance for patients with rheumatic and musculoskeletal diseases receiving immunosuppressive therapy, including biological agents and disease-modifying anti-rheumatic drugs [22].
COVID-19 can cause viral Pneumonia. This patient showed no evidence of Radiographic Viral Pneumonia or increased biomarkers. In addition, COVID-19 can cause myocardial damage and Myocarditis. This patient’s echocardiogram showed no evidence of myocardial impairment and Troponins and BNP were negative for myocardial injury during the patient’s hospital course. Also, acute viral infections can be responsible for Acute Coronary Syndrome, and plaque rupture can trigger and precipitate Acute Coronary Syndromes and plaque rupture, but this was not demonstrated in this case [23]. It appears the patient developed an abrupt, overwhelming, acute Respiratory Distress Syndrome, which came on precipitously as a result of the virus in a very immunocompromised host.

Figure: A recent JAMA Cardiology article published the above chart indicating the potential mechanisms for acute effects of viral infections on the Cardiovascular system [23, JAMA Cardiol. Published online March 27, 2020. doi:10.1001/jamacardio.2020.1286]. The pathway outlined in red represents the patient in this case study.
CONCLUSIONS:
We believe this to be a landmark case and we discuss recommendations for expanded guidelines. To this end we present a patient with IMNM who required aggressive immunosuppressive therapy because of acute relapse and significant progression of dysphagia. Unexpectedly, the patient had an acute cardio-hypoxemic episode with cardiopulmonary arrest which was terminal. He had no significant symptoms or radiographic consistent with COVID-19 acute infection. He may have developed the infection while in the hospital, but this is uncertain. We propose that rheumatological patients, even when asymptomatic, be tested for COVID-19 prior to initiating second-line immunosuppressive therapy treatment.
REFERENCES
__________
[1] Five or six hours after workout, the decreased body core temperature signals the body to sleep, promoting less time to fall asleep and sounder sleep cycles, resulting in more restorative sleep and less daytime drowsiness. Also, since Exercise helps to reduce body weight (see below), less weight may mean less risk of Sleep Apnea and snoring.
[2] Exercise increases circulation, thereby increasing tissue oxygenation and removal of wastes from throughout the body (detoxifies). In the brain, this improves function, including concentration, creativity, and productivity. In addition to an improved cardiovascular system, the endorphins released stimulate the mind for more creative thoughts.
[3] “Too busy” is a logical excuse to skip a work out, but physical activity actually helps alleviate stress and promotes productivity. Exercise increases the body’s ability to handle stress. It produces higher levels of norepinephrine, a chemical that regulates areas of the brain that send stress signals. The more the body is trained with the healthy physical stresses of mild to moderate exercise, the better the body responds to emotional and mental (as well as physical) stresses.
[4] Through aging, brainpower decreases and the brain actually grows smaller. Mental decline can start as early as 24 years of age. The elderly who exercise show less brain shrinkage than those who do not. Therefore, exercise may also reverse brain shrinkage. Regular physical activity (3 to 5 times a week for 30 to 60 minutes) helps maintain or sharpen thinking, learning, and judgment skills with age, and increases memory by increasing the volume of gray matter in the brain.
[5] The P&S (autonomic) nervous systems control and coordinate all of the organs and “involuntary” functions of the body. A proper balance is needed, both at rest and during activity. Note, sleeping is an activity and so is sitting at a desk and working, but sitting watching television is not. Exercise by itself can balance the P&S nervous systems better than any supplement or diet alone. Again, the best is when exercise and diet and the rest of the Mind-Body Wellness Program are taken together! Establishing and maintaining P&S balance should always be a goal, and mild to moderate exercise (at a minimum) is an excellent adjunct to pharmacology and other lifestyle measures, including diet in this regard.
[6] Exercise reduces stress, reducing cortisol levels (as mentioned above), psycho-social stress, anxiety, depression (as mentioned above), and fatigue. It reduces oxidative stress, improving endothelial function, increasing nitric oxide production, and the numbers of mitochondria for more energy.
[7] Physical activity engages the entire body, and a healthier cardiovascular system means the heart is better able to circulate blood to all parts of the body, including in older individuals. Heart disease and stroke are two of the leading causes of death in the United States. Following physician recommendations and getting at least 150 minutes a week (2½ hours) of moderate-intensity activity reduces the risk for these diseases. The more (mild to moderate) exercise, the more that risk is reduced. Regular physical activity improves almost all cardiac risk factors, including by increasing HDL cholesterol, lowering LDL cholesterol (clears arteries), lowering blood pressure, increasing cardiovascular fitness, and making the blood less prone to thrombosis or clotting, not only around the heart but also in the brain. Greater blood flow to the brain underlies the brain function improvements mentioned above, including: restorative sleep, improves mood, reduces depression, helps clear “brain fog,” improves cognitive abilities, and perhaps memory.
[8] Exercise reduces cortisol release for better neuroendocrine balance. It helps to keep insulin levels healthy and increases insulin sensitivity. It boosts sex hormones. It helps to maintain healthy thyroid and hypothyroid hormone levels, including levels of growth hormones, which in adults helps with healing and repair.
[9] Diet and physical activity play a critical role in weight management. Weight gain occurs when the calories burned, including those burned during physical activity, are less than the calories consumed. The amount of physical activity required for weight management varies greatly, depending on metabolism (genetics), age (including stage of development), environment, and more. Physical activity can help with weight loss as well as weight maintenance. Establishing and maintaining a healthy weight requires both regular physical activity and a healthy eating plan.
[10] Regular physical activity reduces risk of developing type 2 Diabetes and Metabolic Syndrome. Metabolic Syndrome includes a combination of (1) too much fat around the waist, (2) high blood pressure, (3) low HDL cholesterol, (4) high triglycerides, or (5) high blood sugar. Lower rates of these conditions are seen with 120 to 150 minutes (2 to 2½ hours) a week of mild to moderate-intensity aerobic activity. The more exercise, the more the risk is reduced (to a limit – see your doctor). Regular physical activity also helps control blood glucose levels and can reverse type 2 Diabetes and Metabolic Syndrome.
[11] Regular physical activity reduces risk of cancers as compared with people who do not exercise regularly. Physically active people have a lower risk of colon cancer. Physically active women have a lower risk of breast cancer. Regular physical activity reduces risk of endometrial and lung cancer. Improve quality of life. Cancer survivors who exercise regularly have improved quality of life and physical fitness over those who do not.
[12] Bones and joints, as well as muscles, change with activity level and age. They also need more protection with age. Physical activity strengthens them, which protects bones and joints. Strong and healthy bones, joints, and muscles promote an active lifestyle. Adding a proper diet ensures the necessary micronutrients to maintain bone, joint, and muscle health. Physical activity of at least a moderately-intense level slows the loss of bone density that comes with age. Altogether, exercise helps to reduce the risk of falling in elderly, either due to fewer leg bone fractures or improved muscle strength. Hip fracture is a serious health condition that often negatively affects quality of life, especially for older adults (e.g., climbing stairs, grocery shopping, or playing with the children or grandchildren). However, 2 to 5 hours of at least moderate-intensity aerobic activity each week lowers risk of hip fracture.
Regular physical activity reduces risk of developing, and helps to manage, arthritis and other joint disorders. For arthritis, 2 to 2½ hours a week of moderate-intensity, low-impact activity improves the ability to manage pain and do everyday tasks, and improves quality of life, not just from the pain, but also in terms of range of motion.
Muscle-strengthening activities help increase or maintain muscle mass and strength. Gradually increasing the amount of weight and number of repetitions provides even more benefits, including endurance, no matter the age. Regular physical activity helps to return and improve quality of life, reduces morbidity risk (including dizziness and lightheadedness, thereby reducing fall risk), and mortality risk, at any age.
[13] Exercise alone has never been proven to increase longevity. However, by reducing mortality risk, increasing the antioxidant milieu, boosting immune activity, reducing stress (including pain), and maintaining nervous system and cardiovascular health (establishing and maintaining P&S balance and Mitochondrial health in support of wellness), a patient’s natural longevity is promoted or preserved. Only a few lifestyle choices have as large an impact on health as physical activity. People who are physically active for about 7 hours a week have a 40% lower risk of dying early than those who are active for less than 30 minutes a week; and this activity does not have to be vigorous; moderate-intensity is sufficient. Everyone may gain the health benefits of physical activity. Age, ethnicity, shape, or size does not matter. One hundred and fifty minutes of moderate exercise per week (approximately 21 minutes per day) is routinely advocated for patients.
[14] DePace NL, Colombo J. Autonomic and Mitochondrial Dysfunction in Clinical Diseases: Diagnostic, Prevention, and Therapy. Springer Science + Business Media, New York, NY, 2019.
[15] Dalakas MC. Inflammatory Muscle Diseases. N Engl J Med. 2015 Jul 23; 373(4): 393-4. doi: 10.1056/NEJMc1506827.
[16] Basharat P, Christopher-Stine L. Immune-Mediated Necrotizing Myopathy: Update on Diagnosis and Management. Curr Rheumatol Rep. 2015 Dec;17(12):72. doi: 10.1007/s11926-015-0548-6.
[17] McGrath ER, Doughty CT, Amato AA. Autoimmune Myopathies: Updates on Evaluation and Treatment. Neurotherapeutics. 2018 Oct;15(4):976-994. doi: 10.1007/s13311-018-00676-2.
[18] Marie I, Ménard JF, Hachulla E, et al. Infectious complications in polymyositis and dermatomyositis: A series of 279 patients. Semin Arthritis Rheum. 2011; 41(1): 48–60. doi: 10.1016/j.semarthrit.2010.08.003. Epub 2010 Nov 2.
[19] Singhal T. A Review of Coronavirus Disease-2019 (COVID-19). Indian J Pediatr. 2020 Apr; 87(4): 281-286. doi: 10.1007/s12098-020-03263-6. Epub 2020 Mar 13.
[20] McIntosh K. Coronavirus disease 2019 (COVID-19) – Update. March 2020; https://www.uptodate.com/contents/coronavirus-disease-2019-covid-19.
[21] Hospital for Special Surgery: What to know about Rheumatic Diseases and the COVID-19 coronavirus, published March 11, 2020, access March 13, 2020, https://www.hss.edu/conditions_ rheumatic-disease-and-COVID-19-coronavirus. asp
[22] European League Against Rheumatism (EULAR). EULAR Guidance for patient’s COVID-19 outbreak. Accessed March 13, 2020 www.eular.org/eular_guidance_for_patients_covid19_outbreak.cfm.
[23] Madjid M, Safavi-Naeini P, Solomon SD, Vardeny O. Potential Effects of Coronaviruses on the Cardiovascular System: A Review. JAMA Cardiol. Published online March 27, 2020. doi:10.1001/jamacardio.2020.1286