Click Here to Download this Blog Post – More Than Just “Bendy”: The Hidden Link Between Flexible Joints and Dizzy Spells (Part 8)
By Dr. Nicholas L. DePace, M..D., F.A.C.C – Cardiologist specializing in autonomic dysfunction, Ehlers-Danlos syndrome and POTS.
More Than Just “Bendy”: The Hidden Link Between Flexible Joints and Dizzy Spells
If you are a young woman who has spent years visiting doctors for chronic pain, overwhelming fatigue, and a racing heart every time you stand up, you might feel like you are chasing a mystery. You might have been told you are “just anxious,” or perhaps you’ve been diagnosed with Fibromyalgia.
But what if your loose joints and your dizzy spells are actually part of the same picture?
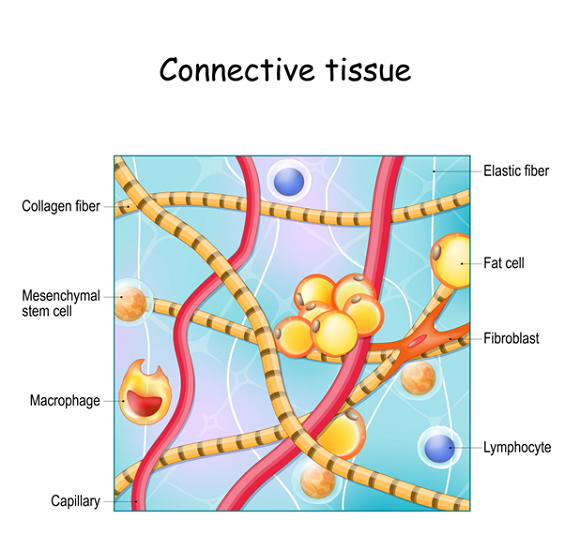
For many patients, the answer lies in hEDS (Hypermobile Ehlers-Danlos Syndrome) or HSD (Hypermobility Spectrum Disorder). While these conditions are defined by connective tissue, the hallmark sign that often leads to a diagnosis isn’t just double-jointedness—it is a dysfunction of the nervous system.
The “Check Engine Light” of the Body
When patients come to our clinic, they often present with a specific collection of struggles:
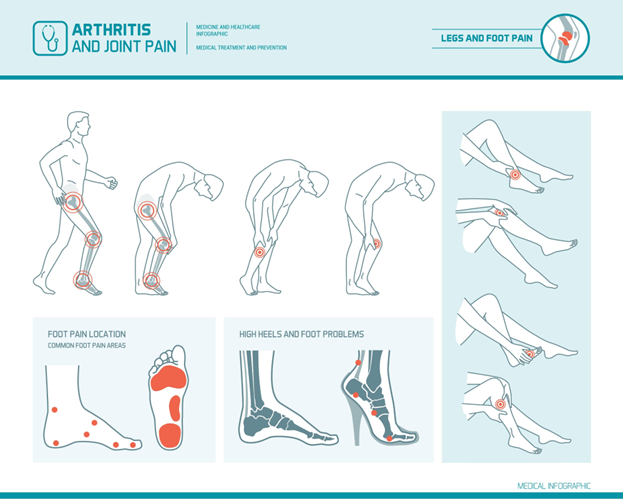
- Chronic Pain and stiff joints.
- Easy Bruising (skin that marks easily).
- Chronic Fatigue that sleep doesn’t seem to fix.
- Orthostatic Dysfunction (getting dizzy, seeing stars, or fainting when standing up).
- Racing Heart Rate (consistent with POTS – Postural Orthostatic Tachycardia Syndrome).
- Temperature issues (sweating too much or overheating easily).
While hEDS is a connective tissue disorder, nearly 100% of the patients we see also have issues with their Autonomic Nervous System (the automatic system that controls heart rate, digestion, and blood pressure).
Key Insight: We often discover the hypermobility because we are investigating the dizziness and heart rate issues. The loose joints are essentially predisposing the body to these nervous system glitches.
Connecting the Dots: The P&S Rollercoaster
To understand why you feel this way, we have to look at the two branches of your autonomic nervous system: the Parasympathetic (Rest and Digest) and the Sympathetic (Fight or Flight).
In hEDS/HSD patients, these two systems are often out of sync:
- Sympathetic Withdrawal: When you stand up, your “Fight or Flight” system should activate slightly to push blood to your head. In hEDS, this response is often weak (withdrawal). This leads to Orthostatic Dysfunction—dizziness and POTS.
- Parasympathetic Excess: The “Rest and Digest” system overcompensates. While this sounds calm, too muchactivity here causes problems like fainting (Syncope), stomach issues (GI motility disorders), inflammation, and an amplification of pain and anxiety.
The Fibromyalgia Confusion
A significant number of patients—at least one-third—come to us with a previous label of Fibromyalgia.
It is easy to see why: both conditions cause widespread pain and fatigue. However, in many cases, the root cause isn’t Fibromyalgia; it is hEDS/HSD causing joint instability and nervous system dysfunction. Recognizing the difference is vital for getting the right treatment.
hEDS vs. HSD: What’s the Difference?
- hEDS (Hypermobile Ehlers-Danlos Syndrome): This is the most common connective tissue disorder seen in clinics. It has a suspected inheritance pattern (autosomal dominant), meaning it runs in families, though the specific gene hasn’t been identified yet.
- HSD (Hypermobility Spectrum Disorder): Think of this as the sibling to hEDS. A person has the symptoms (pain, hypermobility) but might miss the strict criteria for hEDS by a point or two. Genetic understanding here is even scarce, but the management is largely the same.
Safety First: Ruling Out the “Scary” Stuff
Because hEDS is part of a larger family of tissue disorders, doctors must perform a Differential Diagnosis. This means running tests to rule out rare, life-threatening conditions like Marfan syndrome, Vascular EDS (vEDS), or Loeys-Dietz syndrome.
These rare conditions affect the aorta and blood vessels. However, for the vast majority of patients (98%+), these are ruled out, leaving us with the hEDS or HSD diagnosis.
The Good News
While living with hEDS/HSD can be exhausting and painful, the prognosis is favorable. Unlike the rare vascular types, hEDS/HSD is associated with a normal life expectancy.
Understanding that your racing heart, your anxiety, your tummy troubles, and your joint pain are all connected is the first step toward management. You aren’t “just anxious” and you aren’t imagining it. It is a systemic connection between your tissues and your nerves, and it can be managed.
It is important to seek out a clinician with expertise in EDS to make an accurate diagnosis and create a treatment plan. One of the nation’s leading centers is Franklin Cardiovascular Associates, under the direction of Nicholas DePace, MD, FACC. They are located in Sicklerville, New Jersey. franklincardiovascular.com, (856) 589-6034.
It is important to seek out a clinician with expertise in EDS to make an accurate diagnosis and create a treatment plan. One of the nation’s leading centers is Franklin Cardiovascular Associates, under the direction of Nicholas DePace, MD, FACC. They are located in Sicklerville, New Jersey. franklincardiovascular.com, (856) 589-6034
About the Author
Nicholas L. DePace, MD, FACC is a board-certified cardiologist and Medical Director of Franklin Cardiovascular Associates. A graduate of the Mount Sinai School of Medicine, Dr. DePace has decades of clinical, academic, and research experience and has held faculty appointments as a Clinical Professor of Medicine, becoming one of the youngest full professors in Philadelphia at the time of his appointment.
Dr. DePace specializes in the diagnosis and treatment of autonomic nervous system dysfunction (dysautonomia), including POTS, autonomic dysfunction associated with Ehlers-Danlos syndrome (EDS), chronic fatigue, and anxiety-like conditions that are frequently misdiagnosed. He is nationally recognized for his work on parasympathetic and sympathetic (P&S) nervous system imbalance, a core mechanism underlying many complex chronic disorders.
In addition to treating patients from across the United States, Dr. DePace is a prolific clinical researcher and author of multiple nationally distributed medical textbooks published by Springer and W.W. Norton, focusing on autonomic dysfunction, mitochondrial disorders, cardiovascular disease, and mind–body medicine.
👉 View Dr. DePace’s professional profile
👉 View medical books by Dr. DePace